Want to improve athletic performance? Find your personalized eating plan. Avoid the foods you do not tolerate.
FOOD INTOLERANCE IS A RAPIDLY INCREASING PROBLEM THAT DIFFERS FROM FOOD “ALLERGY” IN THAT SYMPTOMS ARE USUALLY CHRONIC AND DELAYED, PERHAPS BY SEVERAL HOURS OR EVEN DAYS. HENCE THEY HAVE RECEIVED RELATIVELY LITTLE ATTENTION. NONETHELESS, KNOWING WHAT FOODS YOU DO NOT TOLERATE MAY BE THE MOST POWERFUL TOOL FOR IMPROVING ATHLETIC PERFORMANCE AND WELL BEING.
Ask many of the top professional and amateur athletes what their training secret is and they will respond by saying, “Personalized eating!”
 Eating healthful food is one thing, but eating in accordance with your own unique, genetically determined biochemical makeup is quite another thing. One man’s meat is another man’s poison. Finding out what foods are right (and which are wrong) for you is the key to health and performance.
Eating healthful food is one thing, but eating in accordance with your own unique, genetically determined biochemical makeup is quite another thing. One man’s meat is another man’s poison. Finding out what foods are right (and which are wrong) for you is the key to health and performance.
Foods that are compatible with your make up will increase your strength and energy. Consumption of foods or added chemicals that YOUR body perceives as harmful will result in intolerance reactions. Food intolerance induces the excessive generation of toxic free radicals and inflammatory chemicals. The damage can result in a wide range of health problems. The following are some of the effects of food intolerance that are of strong interest to athletes:
1. Direct damage to the mitochondria in our cells. The mitochondria are the sites where energy is produced. The wrong food activates the immune system and free radicals and attacking molecules produced can cause damage to the DNA, and other structures within the mitochondria, resulting in lower energy production. This is of special significance to athletes because intense exercise alone will generate damaging free radicals from the normal metabolic process, sped up somewhat by the intensity of the exercise. Usually, this is not a problem if your anti-oxidant enzymes and nutritional anti-oxidants are sufficient. Complicate it with food intolerance and the generation of free radicals will overload your systems.
2. Related in some ways to this is that inflammation will also cause a shortening of the ends of the strands of your DNA, called telomeres. Telomeres are like the plastic pieces at the end of a shoe lace, holding the DNA strands together. Whenever the cell divides, and immune cells divide frequently, the telomeres are shortened. When they become too short the cell can no longer reproduce; it becomes old and dies. This could explain cancer and generalized weakened immunity in old age. Avoid this by avoiding inflammation. We can choose what we eat.
3. Auto-immunity can also arise from too much inflammation. Some immune cells die in the process of trying to neutralize a food. The DNA from the dead cells release their own genetic material, which, if the amount is too great, may be perceived as “foreign” bodies the immune system must attack. However, this time you are attacking the blueprint for your own bodily proteins (structures) and auto-immune reacts may occur. Again, it’s better to avoid this if you can.
4. Certain immune chemicals with names like Interleukin 6 and tumor necrosis factor alpha will block insulin receptors on your muscle (and brain and liver) cells. This is a recently discovered finding made by medical scientists that explains why food intolerance makes people fat. The muscle cells are starved of important energy material which is instead stored as fat in fat cells.
5. Food intolerance can cause inflammation in the gut. An extreme form is celiac disease. This reduces the absorption of nutrients that are needed for proper energy production as well as all other biological processes. It also consumes serotonin in the gut. Serotonin deficits are related to sugar craving.
6. Toxic immune chemicals such as elastase damage muscle tissue.
7. Food intolerance can cause inflammation in the upper and lower airways. Decreased air intake limits aerobic metabolic function.
8. Chronic inflammation also makes you fatigued. Ever wonder why you feel so tired when you get the flu? It’s because the same immune chemicals that are intended to fight viruses cause fatigue, so you are forced to rest when you are sick. Your body wants you to rest, not exercise, so that your energy can be used to fight the invader. The immune system that’s inappropriately activated by the wrong food will thus cause you to be chronically fatigued to a lesser or greater extent. The immune system is now mistaking a food particle for a virus or bacterium.
In contrast with “True” allergy, whereby a few molecules of peanut may, for example, induce anaphylaxis, the sheer magnitude of exposures to intolerogenic foods, despite it’s less dramatic flare (pun intended) render FOOD INTOLERANCE FAR MORE COMMON.
Allergy vs. Intolerance
The biological cause of true allergy has been known since 1967. An immune system structure called IgE plays a central role. A small amount of allergen, interacting with IgE, can trigger the release of chemicals that create allergic symptoms. Many people react to animals, pollens, and, in rare, unfortunate cases, foods.
Food allergy symptoms are quite dramatic, and intentionally so, as this pathway represents our natural defense against large parasites, like helminths. Unlike other pathogens (i.e. viruses and bacterium) these parasitic worms are significantly larger than the cells that protect against them. Hence, our immune defense must be very strong, which is why allergies produce such dramatic symptoms.
In contrast, intolerances to foods follow different pathways, and symptoms are dose related, chronic and delayed. Consequently, most people are unaware of their food intolerances.
:dropcap_open:When chemicals in foods (naturally occurring or otherwise) cannot be adequately detoxified by the liver, the immune system is called to action.:quoteleft_close:
Offending food may be tolerable until such time as a chemical naturally occurring within the food, or that has been added, exceeds a certain threshold. Many athletes are consuming energy bars that are complex. The modern diet is, in general, very complex and certainly not what our ancestors had been exposed to for sufficient time for us to adapt. Hence, even “normal” foods may be simply unfamiliar to us, from a genetic point of view, and aggravate the immune system.
Another consequence of the modern diet is that nutritional cofactors required for hepatic biotransformation are lower in commercially-grown produce. When chemicals in foods (naturally occurring or otherwise) cannot be adequately detoxified by the liver, the immune system is called to action.
This “total load” is further impacted by the integrity of the gut membrane which, under normal circumstances, forms a natural barrier. Infection, an imbalance in gut flora, antibiotics, cortisone (exogenous or endogenously produced by excessive stress) and hormones used in birth control, compromises the gut barrier.
Classical, or IgE, allergy to food has been recognized for centuries. The first recorded anaphylactic reaction to eggs occurred in the sixteenth century (1) and a fish-induced allergy was reported in the seventeenth century. However, the more recent development of other non-allergic adverse reactions to foods, including food intolerance, only began receiving recognition following the work of Chicago-based allergist Theron Randolf in the 1950s (3).
Modern agriculture causes modern diseases, inflammation
The link between food intolerance, chemical sensitivity and the dramatic increase in degenerative diseases is clear; coinciding, as they do, with consumption of junk food. When low quality and non-compatible foods are avoided, inflammation resolves, weight normalizes, and a number of other inflammatory-based health problems subside.
As seen from this necessarily simplified analysis, adverse food reactions may be toxic or nontoxic reactions. Toxic reactions occur in anyone, given sufficient exposure. Nontoxic reactions occur in susceptible individuals and may result from chemicals occurring in aged cheese or chocolate; and may involve either immune mechanisms (allergy or hypersensitivity) or non- immune mechanisms. The former are referred to as “hypersensitivities”, the latter, “intolerances”.
Food intolerances are the most common. They are most likely caused by the pharmacologic activities of chemicals that naturally occur in the food, or those that are added to the food.
However, some intolerance results from inherited enzyme deficiencies, and thus remain fixed. Some reactions are exacerbated by poor digestion related to intestinal disorders, or the overwhelming of specific detoxification pathways, that are rate limited (4). Hence, addressing these underlying issues can result in tolerance of moderate quantities of the food.
Because numerous and varied mechanisms play a role in the pathogenesis of adverse reactions to foods, definitive identification of offending foods relies upon provocation of symptoms following oral challenge under double-blind conditions—not always a convenient option for a training athlete. Various serum tests exist but are of questionable value. Whereas testing serum levels of allergen-specific IgE is a useful test for classical allergy, it is of limited value for identification of foods and chemicals associated with intolerance that are not IgE mediated. Rather, a useful test for intolerances would have to measure the direct effect of the food substance on the very immune system cells that are responsible for these intolerances. It should show a good correlation with clinical symptoms, as confirmed by double-blinded oral challenges. The only test meeting these criteria is the Alcat test. The Alcat test was developed by scientists working in the US in the mid ‘80s. It has since spread throughout the world and is now available in Germany. It has begun to start a revolutionary breakthrough in sports and general medicine that many have not yet come to terms with. However, its many benefits are well documented.
Other Manifestations
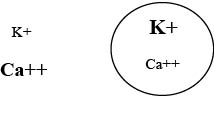
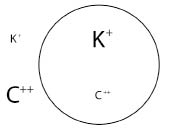
Previously, childhood diabetes was exclusively of the Type 1, auto-immune based type. The consequence: high blood sugar levels and tissue degeneration. Perhaps this is just the tip of the iceberg. Now, due to over activation of the innate immune system, due to food intolerance, so called “adult onset” diabetes occurs even in children. Adult onset diabetes is not auto-immune per se, but occurs when insulin receptors on muscle, the liver and the brain lose effectiveness. Insulin resistance is the hallmark of metabolic syndrome. Initially, insulin is produced, but it cannot sufficiently facilitate the uptake of glucose because of the insensitivity of the insulin receptors. The pancreas then produces increasing quantities of insulin but of lower quality. Blood sugar levels increase.
Interleukin 6 and tumor necrosis factor alpha block insulin receptors. Glucose is stored in adipocytes (fat cells) which in turn produce these very same mediators perpetuating the cycle of inflammation, muscle degeneration and inefficient metabolism.
Solutions
The foremost approach to achieving health, leanness and improved energy and strength should be dietary; emphasizing healthy, natural, nutritious food along with exercise, stress management, intestinal health and adequate nutrition.
Foods that act as triggers require proper identification and avoidance. Testing of white blood cell reactions is the best approach. It reflects pathological responses to foods that are mediated by immunologic, non-immunologic, pharmacologic as well as toxic pathways. The Alcat test is a scientifically validated approach that exhibits the highest degree of correlation with blinded challenges and is the most accurate (5). Symptom resolution, normalization of weight and broad clinical correlation affirm this as a most beneficial tool to be added to any health and sports regimen (6).
Roger Davis Deutsch founded Science Systems Corp (CSS), located in Deerfield Beach, FL. CSS developed The ALCAT Test to determine intolerances to foods, additives, environmental chemicals, molds, drugs and other substances. He began his involvement of development in food intolerance and other Alcat technology-based tests in 1986. He may be reached at Cell Science Systems, Corp., 852 S. Military Trail, Deerfield Beach, FL 33442 or [email protected].
REFERENCES
1. Cohen SG, Saavedra-Delgado AM. Through the centuries with food and drink, for better or worse II. Allergy Proc 1989; 10:363-73.
2. Harper DS. Egg?—Ugh! In: Avenberg KM, editor. Footnotes on Allergy. Uppsala: Upplands Grafiska AB; 1980. p. 52.
3. Bruijnzeel-Koomen C, Ortolani C, Aas K, et al. Adverse reactions to food allergy. 1995; 50:623-35.
4. Deutsch, R. The Right Stuff: Use of Alcat testing for determining dietary factors effecting immune balance, health and longevity. Anti-Aging Therapeutics. Chapt. 9, Vol. 10, 2007
5. Høj, L. Diagnostic value of ALCAT test in intolerance to food additives compared with double blind placebo controlled (DBPC) oral challenges. Alleg Clin Immun 1996: No 1, part 3.
6. Brostoff, J., et. al., 45th An. Congress, Am. Col. of Allergy & Imm.
 The Pathophysiology of Metabolic Syndrome
The Pathophysiology of Metabolic Syndrome

 :dropcap_open:S:dropcap_close:ome health problems are purely genetic. Others have nothing to do with genetics but are purely the result of environmental influences, such as diet, infection, or trauma. Then, there are many conditions in which some genetic predisposition interacts with the environment to produce the disease. The classic example is celiac disease, which is tightly linked to genetics but can be controlled by eliminating wheat, rye, and barley products from the diet. Considerable evidence suggests that many of the inflammatory arthritides, including ankylosing spondylitis, could also respond to dietary interventions, including a low-fat, purely plant-based (vegan) diet or sometimes a gluten-free diet.
:dropcap_open:S:dropcap_close:ome health problems are purely genetic. Others have nothing to do with genetics but are purely the result of environmental influences, such as diet, infection, or trauma. Then, there are many conditions in which some genetic predisposition interacts with the environment to produce the disease. The classic example is celiac disease, which is tightly linked to genetics but can be controlled by eliminating wheat, rye, and barley products from the diet. Considerable evidence suggests that many of the inflammatory arthritides, including ankylosing spondylitis, could also respond to dietary interventions, including a low-fat, purely plant-based (vegan) diet or sometimes a gluten-free diet. An intriguing case report from Germany suggests that a vegan diet (i.e., a diet that excludes foods of animal origin) holds promise for patients with ankylosing spondylitis.6 The report describes a 33-year-old patient who inherited an HLA-B*27 from both parents and had a 10-year history of ankylosing spondylitis that had responded poorly to conventional medical treatment and physiotherapy. The authors recommended that the patient switch temporarily to a purely vegan diet, avoiding all animal fats and proteins. The patient’s symptoms started to improve within 3 to 4 days after the switch to a vegan diet. After the patient resumed eating meat 6 weeks later, the condition started to worsen again. The patient then resumed the vegan diet. At 3 months’ follow-up, the patient had quit taking tramadol and ibuprofen, had cut his meloxicam dose in half, and was “almost completely free of complaints.”
An intriguing case report from Germany suggests that a vegan diet (i.e., a diet that excludes foods of animal origin) holds promise for patients with ankylosing spondylitis.6 The report describes a 33-year-old patient who inherited an HLA-B*27 from both parents and had a 10-year history of ankylosing spondylitis that had responded poorly to conventional medical treatment and physiotherapy. The authors recommended that the patient switch temporarily to a purely vegan diet, avoiding all animal fats and proteins. The patient’s symptoms started to improve within 3 to 4 days after the switch to a vegan diet. After the patient resumed eating meat 6 weeks later, the condition started to worsen again. The patient then resumed the vegan diet. At 3 months’ follow-up, the patient had quit taking tramadol and ibuprofen, had cut his meloxicam dose in half, and was “almost completely free of complaints.”
 According to Dr. Carolyn Dean, MD, ND, magnesium expert and Medical Director of the nonprofit Nutritional Magnesium Association (
According to Dr. Carolyn Dean, MD, ND, magnesium expert and Medical Director of the nonprofit Nutritional Magnesium Association (
 Eating healthful food is one thing, but eating in accordance with your own unique, genetically determined biochemical makeup is quite another thing. One man’s meat is another man’s poison. Finding out what foods are right (and which are wrong) for you is the key to health and performance.
Eating healthful food is one thing, but eating in accordance with your own unique, genetically determined biochemical makeup is quite another thing. One man’s meat is another man’s poison. Finding out what foods are right (and which are wrong) for you is the key to health and performance.

 :dropcap_open:T:dropcap_close:his article is the conclusion of a series on the short leg syndrome. Previously, I have discussed the importance of proper alignment of the hip, knee, and ankle joints to each other. This month, we move into the pelvis and summarize the role of proper lower extremity mechanics on walking and maintaining proper spinal alignment.
:dropcap_open:T:dropcap_close:his article is the conclusion of a series on the short leg syndrome. Previously, I have discussed the importance of proper alignment of the hip, knee, and ankle joints to each other. This month, we move into the pelvis and summarize the role of proper lower extremity mechanics on walking and maintaining proper spinal alignment. 
 :dropcap_open:Y:dropcap_close:ou know the food you’re eating is bad for you—you just can’t stop eating it. You have a food addiction and you’re not alone. Millions of people are suffering as well.
:dropcap_open:Y:dropcap_close:ou know the food you’re eating is bad for you—you just can’t stop eating it. You have a food addiction and you’re not alone. Millions of people are suffering as well.
 :dropcap_open:L:dropcap_close:ast month, I started a three-part series on the short leg syndrome and the absolute necessity of not only properly identifying it, but finding the exact cause, and tracing the effects up the leg into the pelvis and onto the spine.
:dropcap_open:L:dropcap_close:ast month, I started a three-part series on the short leg syndrome and the absolute necessity of not only properly identifying it, but finding the exact cause, and tracing the effects up the leg into the pelvis and onto the spine.


 :dropcap_open:T:dropcap_close:his month, I begin a series of 24 articles each designed to highlight a set of symptoms that collectively point at a specific visceral problem that is perpetuating muscle contractions, loss of joint range of motion, and reoccurring structural misalignments that have become chronic and defy permanent correction. It is exactly these problems that cause patients to seek alternatives to continuing chiropractic care. I believe our profession must, in addition to specializing in structural disorders, begin identifying these underlying visceral problems and specialize in restoring normal function before disease entities can be identified.
:dropcap_open:T:dropcap_close:his month, I begin a series of 24 articles each designed to highlight a set of symptoms that collectively point at a specific visceral problem that is perpetuating muscle contractions, loss of joint range of motion, and reoccurring structural misalignments that have become chronic and defy permanent correction. It is exactly these problems that cause patients to seek alternatives to continuing chiropractic care. I believe our profession must, in addition to specializing in structural disorders, begin identifying these underlying visceral problems and specialize in restoring normal function before disease entities can be identified.
 While all of this may seem inconsequential in a structural practice, it does result in an inability to respond appropriately to parasympathetic stimulation with an apparent sympathetic dominance and the symptoms of Fright-Fight-Flight are well documented. Every day, we see patients who are irritable and argumentative, or cannot adequately tolerate stress.
While all of this may seem inconsequential in a structural practice, it does result in an inability to respond appropriately to parasympathetic stimulation with an apparent sympathetic dominance and the symptoms of Fright-Fight-Flight are well documented. Every day, we see patients who are irritable and argumentative, or cannot adequately tolerate stress.