:dropcap_open:T:dropcap_close:he IME, or independent medical examination, and peer review processes are necessary and integral steps in maintaining a system of checks and balances in health care billing in order to prevent unnecessary care. Over the last two decades, the system has evolved to where too many doctors who are hired by the carriers through an IME company (middle man) or directly by the carriers are not performing examinations that are remotely close to independent. Going back 20-30 years, you could historically find inaccuracies in how the insurance companies hired doctors that reported on the conditions of the patients.

In addition, rarely were retrospective audits or retrospective opinions from contemporary IMEs performed or rendered. Today, this has become vogue and a huge revenue source for private, public and governmental carriers alike. There is hardly a doctor in the nation that hasn’t been affected by overwhelming negative IMEs that include inaccuracies, partial truths and a blatant disregard and/or misrepresentation of facts.
Over the years, too many IME companies have handed doctors completed reports, mandated diagnoses, misquoted research and given strict orders regarding the scope of care permitted, all prior to the examination. In almost every instance I have encountered, the carrier or IME company has offered to send the doctor more cases if he/she works with them to reach a desired conclusion, whatever that may be.
Treating doctors currently have 2 choices. They can either ignore the opinions rendered which would tarnish or possibly damage their reputations as treating doctors or fight back with rebuttals. Unfortunately, most doctors choose to do nothing, leaving the final word of their clinical decision making and abilities up to the IME or peer review doctors. For the most part, based upon review of 100s of rebuttals, the doctors who do fight back with rebuttals are fraught with emotional statements and/or attempts to clarify the records.
Although this is a good first step, it comes down to a treating doctor’s word vs. an IME or peer review doctor’s opinion, and in the end the treating doctor rarely wins the argument. If you attempt to scrutinize the reasons why, it comes down to the fact that the IME and peer review processes are time-honored systems for which decades and countless resources have been spent defining templated language and research has often been supplied to the “insurance-hired” doctors. It’s an area where treating doctors do not have access to the same type of technology or research teams that the carriers and the IME companies can afford…and…there is nothing wrong with that.
They just play the game at a higher level than you in order to keep their money…and…it is always about the money. The problem arises when the IME and peer review doctors step over the line of integrity and report partial truths and/or half truths, making glaring omissions, or simply are dishonest in reporting their findings. This is what needs to be focused on in “weeding out the bad ones” and setting the record straight.
Treating doctors are not powerless, but need to understand how to get past the rhetoric of a well-constructed IME or peer review report in order to bring out the inaccuracies, partial truths and blatant disregard of facts when those circumstances arise. In the November, 2011 and February, 2012 issues of this journal, I chronicled actions that can be taken by the treating doctors and state organizations. In March and April of 2012, I outlined the perils facing the IME and peer review doctors. You must first understand every aspect of the process in order to prevent having negative IMEs and peer reviews and prevail in overturning improper reports.
In order to craft a proper rebuttal, it is necessary that you understand the licensure standards of the doctor-patient relationship between the insurance-hired doctor and the patient. You also must understand the regulatory requirements in that examination and the IME or peer review doctor’s requirements to report the results. This is a state by state issue, as each state has independent rules on the required conduct of insurance-hired doctors. You then must learn how to recognize when a partial truth or “untruth” is being documented by the examining doctor. It is that scenario which mandates that you protect both your reputation and your patient’s interests by rendering evidence of how licensure and regulatory standards were not adhered to.
The language typically written by IME doctors is, “The above captioned claimant is examined in accordance with the restrictive rules concerning an independent medical evaluation. Prior to the evaluation, it was explained to the examinee that this appointment was for the purpose of evaluation only and not for care, treatment or consultation, and, therefore, no doctor-patient relationship would result.” In many states, this statement alone is not consistent with court rulings and regulations and can be considered a licensure violation due to a misrepresentation of the facts. Rendering false reports, or misrepresenting material facts is also considered a licensure violation in many states.
Massachusetts regulations state:
4.06: grounds for disciplinary action
The board may, by majority vote after a hearing conducted in accordance with M.G.L. C. 30a and 801 CMR 1.00 et seq., take disciplinary action against any registered chiropractor who holds a certificate of registration issued pursuant to M.G.L. c. 112, §§ 89 through 97 and 233 CMR 2.00. Grounds for such disciplinary action shall include, but shall not be limited to:
(11) engaging in, authorizing, or aiding or abetting, fraud, misrepresentation or deceit in connection with his or her practice of chiropractic, as defined in 233 CMR 4.10;
(12) making any false statement or misrepresentation of material fact in connection with any application or claim for payment of any health care benefit, as defined in 233 CMR 4.11;
Delaware’s regulation’s state:
Title 24. Professions and occupations
Chapter 17. Medical practice act
Subchapter iv. Disciplinary regulation; proceedings of the board
§ 1731. Unprofessional conduct and inability to practice medicine
(a) A person to whom a certificate to practice medicine in this state has been issued may be disciplined by the board for unprofessional conduct, as defined in subsection (b) of this section, by means of levying a fine, or by the restriction, suspension, or revocation, either permanent or temporary, of that person’s certificate to practice medicine, or by other appropriate action, which may include a requirement that a person who is disciplined must complete specified continuing education courses. The board shall permanently revoke the certificate to practice medicine in this state of a person who is convicted of a felony sexual offense.
(b) “unprofessional conduct” includes but is not limited to any of the following acts or omissions:
(1) the use of any false, fraudulent, or forged statement or document or the use of any fraudulent, deceitful, dishonest, or unethical practice in connection with a certification, registration, or licensing requirement of this chapter, or in connection with the practice of medicine or other profession or occupation regulated under this chapter…
Every state has its own rules that must be adhered to. However, some states have separate rules for IME and peer review doctors.
This is one of many avenues that can be taken to overturn improper IME and peer review reports, but remember, the IME and peer review doctors are entitled to their opinions and you do not have to like them or agree with them. For those honest insurance-hired doctors, the solution is for you to simply write a better, more thoroughly documented accounting of your patient’s problems initially, and then rebut the IME doctor’s opinion with your own documentation or request that your patient get an independent opinion from a doctor of his/her own choosing.
For those insurance-hired doctors who have crossed the line of integrity, the only solution is to use the rules and regulations, through documented proof, of how they violated state licensure standards and the best proof is the insurance company-hired doctor’s own report. Don’t let inaccuracies about your clinical opinions and abilities be the last word.
 Better care for patients. For chiropractors, patient care is the top priority. By continuing your learning through professional development opportunities, you are able to offer better care to your patients. Continuing education ensures that you are knowledgeable about the most recent research and techniques, which can be helpful to your patients and ensure they are receiving the best care available.
Better care for patients. For chiropractors, patient care is the top priority. By continuing your learning through professional development opportunities, you are able to offer better care to your patients. Continuing education ensures that you are knowledgeable about the most recent research and techniques, which can be helpful to your patients and ensure they are receiving the best care available.
 In addition, rarely were retrospective audits or retrospective opinions from contemporary IMEs performed or rendered. Today, this has become vogue and a huge revenue source for private, public and governmental carriers alike. There is hardly a doctor in the nation that hasn’t been affected by overwhelming negative IMEs that include inaccuracies, partial truths and a blatant disregard and/or misrepresentation of facts.
In addition, rarely were retrospective audits or retrospective opinions from contemporary IMEs performed or rendered. Today, this has become vogue and a huge revenue source for private, public and governmental carriers alike. There is hardly a doctor in the nation that hasn’t been affected by overwhelming negative IMEs that include inaccuracies, partial truths and a blatant disregard and/or misrepresentation of facts.

 As a teacher to new members to our profession, I firmly believe it’s necessary to learn our lexicon. This is important not only for historical reasons, but also to understand the present and future debates regarding chiropractic and, more importantly, to add to and access the scientific literature and improve patient care. But in order to debate or utilize published evidence, we must be clear and consistent with the words we use. To my knowledge the most comprehensive work to date on establishing consensus in our profession regarding our terminology was done by Gatterman and Hansen in 1994 (1). In the heroic attempt to bring some order to the chaos, they organized and reported on the work of an international Delphi panel, whereby these leaders offered their conclusions about the various words and definitions we commonly use. I would suggest that as a profession we continue to use the definitions that were crafted at that time until a similar process is undertaken to update them. As such, an adjustment is defined as “ANY (emphasis added) chiropractic therapeutic procedure that utilizes controlled force, leverage, direction, amplitude, and velocity which is directed at specific joints or anatomical regions. Chiropractors commonly use such procedures to influence joint and neurophysiological function.”
As a teacher to new members to our profession, I firmly believe it’s necessary to learn our lexicon. This is important not only for historical reasons, but also to understand the present and future debates regarding chiropractic and, more importantly, to add to and access the scientific literature and improve patient care. But in order to debate or utilize published evidence, we must be clear and consistent with the words we use. To my knowledge the most comprehensive work to date on establishing consensus in our profession regarding our terminology was done by Gatterman and Hansen in 1994 (1). In the heroic attempt to bring some order to the chaos, they organized and reported on the work of an international Delphi panel, whereby these leaders offered their conclusions about the various words and definitions we commonly use. I would suggest that as a profession we continue to use the definitions that were crafted at that time until a similar process is undertaken to update them. As such, an adjustment is defined as “ANY (emphasis added) chiropractic therapeutic procedure that utilizes controlled force, leverage, direction, amplitude, and velocity which is directed at specific joints or anatomical regions. Chiropractors commonly use such procedures to influence joint and neurophysiological function.”
 The AMA’s Code of Medical Ethics, Opinion 10.03, is titled “Patient-Physician Relationship in the Context of Work-Related and Independent Medical Examinations” and outlines a cogent relationship that should exist between both IMEs (independent medical examiners) and IEPs (industry employed physicians). The AMA writes:
The AMA’s Code of Medical Ethics, Opinion 10.03, is titled “Patient-Physician Relationship in the Context of Work-Related and Independent Medical Examinations” and outlines a cogent relationship that should exist between both IMEs (independent medical examiners) and IEPs (industry employed physicians). The AMA writes: Should an independent examining doctor do an improper or fraudulent examination in any of those states, the code of ethics will weigh heavily against them. In states like Alaska, Missouri and Colorado where there is no “duty of care” and it has been determined there is no doctor-patient relationship for independent examining doctors, the Code of Ethics then helps litigators, to some degree, in creating justice for the injured. Furthermore, it can help give direction to creating legislation to overturn the court rulings that currently protect the licenses of IME, IEP and peer review abusers. We must never lose sight of the fact that independent examining doctors have a tremendous personal financial gain to render a desired diagnosis and conclusion and there have to be checks and balances in place to ensure an honest opinion is rendered.
Should an independent examining doctor do an improper or fraudulent examination in any of those states, the code of ethics will weigh heavily against them. In states like Alaska, Missouri and Colorado where there is no “duty of care” and it has been determined there is no doctor-patient relationship for independent examining doctors, the Code of Ethics then helps litigators, to some degree, in creating justice for the injured. Furthermore, it can help give direction to creating legislation to overturn the court rulings that currently protect the licenses of IME, IEP and peer review abusers. We must never lose sight of the fact that independent examining doctors have a tremendous personal financial gain to render a desired diagnosis and conclusion and there have to be checks and balances in place to ensure an honest opinion is rendered.
 The nomenclature utilized in a healing, regulated profession cannot be based upon belief. It must be based upon standards taught in our teaching institutions and verified both by research and in the field daily as practiced by clinicians and evidenced by their results. Having spent the last few years researching chiropractic and related topics and having spoken to many in our teaching institutions, it has become “crystal clear” as to why we have gravitated towards the label “manipulation” as a descriptor of what we do rather than “adjusting.” Until you “read between the lines” and see how we are being seen as a result of the lines being blurred, you will not understand the dilemma the dichotomy of language has created.
The nomenclature utilized in a healing, regulated profession cannot be based upon belief. It must be based upon standards taught in our teaching institutions and verified both by research and in the field daily as practiced by clinicians and evidenced by their results. Having spent the last few years researching chiropractic and related topics and having spoken to many in our teaching institutions, it has become “crystal clear” as to why we have gravitated towards the label “manipulation” as a descriptor of what we do rather than “adjusting.” Until you “read between the lines” and see how we are being seen as a result of the lines being blurred, you will not understand the dilemma the dichotomy of language has created. Furthermore, it appears that these responses may demonstrate the relationship of autonomic responses in association to the particular segment(s) adjusted” (Welsh & Boone, 2008, p. 86). The clear conclusion is that a specific chiropractic adjustment is the reason for the positive outcome.
Furthermore, it appears that these responses may demonstrate the relationship of autonomic responses in association to the particular segment(s) adjusted” (Welsh & Boone, 2008, p. 86). The clear conclusion is that a specific chiropractic adjustment is the reason for the positive outcome. A literature search for “chiropractic adjustment” rendered 596 results without all of them being peer reviewed journals. However, all were specific to chiropractic and each is a building block to grow on. A literature search for “spinal manipulation” rendered 8,145 results, but only 3,518 had “chiropractic manipulation” in the text. There is so much overlap in what we do versus what others do that others often lay claim to chiropractic manipulation results to certify non-chiropractic care. We are empowering other professions that manipulate and the regulators, payors and referrers who utilize the research must get a clearer message for chiropractic to flourish. The results are: we get reimbursed at the lowest level or none at all (i.e. Medicaid), there is ongoing legislation further limiting chiropractic care, we are prevented from participating in too many local, state and Federal programs and we are bypassed in the referral process by well meaning but misinformed referral sources such as primary care physicians who rely on literature for verification of the best referral pathway.
A literature search for “chiropractic adjustment” rendered 596 results without all of them being peer reviewed journals. However, all were specific to chiropractic and each is a building block to grow on. A literature search for “spinal manipulation” rendered 8,145 results, but only 3,518 had “chiropractic manipulation” in the text. There is so much overlap in what we do versus what others do that others often lay claim to chiropractic manipulation results to certify non-chiropractic care. We are empowering other professions that manipulate and the regulators, payors and referrers who utilize the research must get a clearer message for chiropractic to flourish. The results are: we get reimbursed at the lowest level or none at all (i.e. Medicaid), there is ongoing legislation further limiting chiropractic care, we are prevented from participating in too many local, state and Federal programs and we are bypassed in the referral process by well meaning but misinformed referral sources such as primary care physicians who rely on literature for verification of the best referral pathway.
 Experts advise that becoming a practice leader means adopting the following strategies to make your office run more smoothly:
Experts advise that becoming a practice leader means adopting the following strategies to make your office run more smoothly: 
 Over the last sixty years the application of traction (to create decompression) has been perceived as a time-dependant therapy, i.e. the minimal effective dose tends to be seen as durational, or time-dependant. Like manipulation, massage and other passive interventions, several sessions (of whatever duration used) are probably necessary to be most effective and most studies suggest from 3-12 sessions. However, how long those sessions need to be is perhaps open to debate and this article is simply a discussion of that possibility. Few if any research studies have undertaken a minimum-dose control.
Over the last sixty years the application of traction (to create decompression) has been perceived as a time-dependant therapy, i.e. the minimal effective dose tends to be seen as durational, or time-dependant. Like manipulation, massage and other passive interventions, several sessions (of whatever duration used) are probably necessary to be most effective and most studies suggest from 3-12 sessions. However, how long those sessions need to be is perhaps open to debate and this article is simply a discussion of that possibility. Few if any research studies have undertaken a minimum-dose control. When we examine the how and why of axial traction we are faced with several ineffable physiological and anatomical considerations. Why can’t the disc react to unloading in just 1-3 minutes with a substantive, clinically relevant benefit? Since we have no definitive answers we’re left with speculation (and future research), but clinical experience can give us some insight. Presently clinicians practicing the Kennedy Technique have been observing patient responses to very short duration sessions and the preliminary results are not disappointing (unless you really love keeping patients on your table).
When we examine the how and why of axial traction we are faced with several ineffable physiological and anatomical considerations. Why can’t the disc react to unloading in just 1-3 minutes with a substantive, clinically relevant benefit? Since we have no definitive answers we’re left with speculation (and future research), but clinical experience can give us some insight. Presently clinicians practicing the Kennedy Technique have been observing patient responses to very short duration sessions and the preliminary results are not disappointing (unless you really love keeping patients on your table).
 We are great at spreading the word about chiropractic: about how healthy eating habits, regular exercise and chiropractic adjustments will help you live a healthy lifestyle. We are great at educating our patients about how subluxation complexes can lead to degeneration, restricted ranges of motion and pain, just to name a few. It is second nature to educate the patient that neurologically it is “above, down and inside out,” and biomechanically it is from the ground up. That is simple anatomy, physiology and biomechanics. But what if a runner asks you how asymmetrical biomechanics of her gait cycle can cause symptoms of low back pain, mid back pain, neck pain, plantar fascitis, chondromalasia, iliotibial band syndrome, tibial stress syndrome or greater trochanteric bursitis? Or better yet, if she has no signs or symptoms, could you tell her why she needs chiropractic care?
We are great at spreading the word about chiropractic: about how healthy eating habits, regular exercise and chiropractic adjustments will help you live a healthy lifestyle. We are great at educating our patients about how subluxation complexes can lead to degeneration, restricted ranges of motion and pain, just to name a few. It is second nature to educate the patient that neurologically it is “above, down and inside out,” and biomechanically it is from the ground up. That is simple anatomy, physiology and biomechanics. But what if a runner asks you how asymmetrical biomechanics of her gait cycle can cause symptoms of low back pain, mid back pain, neck pain, plantar fascitis, chondromalasia, iliotibial band syndrome, tibial stress syndrome or greater trochanteric bursitis? Or better yet, if she has no signs or symptoms, could you tell her why she needs chiropractic care?
 These statistics mean there are less chiropractors practicing in both of these states, and as a result the Cleveland Chiropractic College has closed its California division. The question that remains is how do we reverse this trend? Recently, in a conversation with a chiropractic college administrator, I heard that if the leadership in our profession was more pro-active and we had read the signs 20 years ago, chiropractic would be in a better place. I agree.
These statistics mean there are less chiropractors practicing in both of these states, and as a result the Cleveland Chiropractic College has closed its California division. The question that remains is how do we reverse this trend? Recently, in a conversation with a chiropractic college administrator, I heard that if the leadership in our profession was more pro-active and we had read the signs 20 years ago, chiropractic would be in a better place. I agree.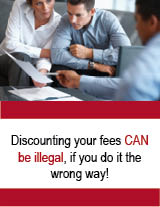
 In the days before insurance, third party reimbursement, state and federal payers, things were simpler. When someone else is paying part or all of the costs for health care, especially the government, rules change and regulations apply. This is when discounting the wrong way can cost you. It’s called doing the right thing the wrong way.
In the days before insurance, third party reimbursement, state and federal payers, things were simpler. When someone else is paying part or all of the costs for health care, especially the government, rules change and regulations apply. This is when discounting the wrong way can cost you. It’s called doing the right thing the wrong way.