Being a principled, subluxation-based or structural-based chiropractor is not mutually exclusive to being responsible for diagnosing your patient accurately. If the patient has a radiculopathic or myelopathic clinical presentation, the question is, “Why?” This has nothing to do with your practice paradigm; it has to do with your patient’s well being and what the cause is for that nerve pressure. There are many etiologies other than subluxation and our job, as chiropractors, is to ensure an accurate diagnosis that allows us to create a successful prognosis and treatment plan.
Based on my experience in the chiropractic setting, approximately 3% of chiropractic patients require referrals for advanced imaging. A July 2009 survey of the profession done by The American Chiropractor indicated that 58.8% of chiropractors order one or less MRI’s per month, suggesting underutilization nationally. As for preference of the type of MRI machine ordered, open, closed or upright, almost 50% have no preference. Only 15% of the profession would prefer neuroradiologists, 85.4% think all imaging companies follow regulatory standards or don’t know and 53.5% think that all types of MRI machines equally detect herniated discs or don’t know.

These results scream out to the profession that we, as a profession, do not understand MRI, a critical practice tool, as much as we need to. In 2009, an integral part of our diagnostic ability is predicated on MRI’s and they are all not alike, nor are MRI companies compelled to follow quality standards, in either performing the test or reporting the results, thereby often rendering blind results with potentially false negatives at the peril of the chiropractor and his/her patients. These false negatives are not a result of the radiologist missing a finding on a film but, many times, result from improper imaging protocols with slices that are “too thick.” Not improper, just clinically non-diagnostic and not regulated.
These false negatives can be eradicated if the chiropractor understands MRI protocols and mandates the correct image sequences and slices in his/her orders. This can only be accomplished with education and it is the responsibility of each individual chiropractor to get the training required to ensure an accurate MRI scan and results. Too many imaging companies, due to economic pressure, will cut corners on these blind items and compromise the results, leaving us in the dark, and that is our fault as much as theirs if we are ignorant.
Many will opine that it is a fault of our professional education that we do not have a greater understanding of MRI and they couldn’t be more wrong. The purpose of our formal education is to give us a starting point to care for our patients and to be able to attain licensure by meeting the minimum national and state standards of practice. It is the responsibility of each individual to then take it to the next level. DD and BJ had the big idea. However, if you study history, you will find that BJ Palmer did more research in concert with his medical counterparts than most, if not all, in contemporary research. He created his own team and maintained control of all chiropractic decisions, as you should.
Twenty years ago when MRI became readily available, there were no courses for chiropractors to learn how to read images and to teach them what protocols to order. I learned how to read the hard way; every time I ordered an MRI, I would go to the radiology office and ask them to show me what they were diagnosing and have them explain the anatomy and the pathology to me. After 100 to 200 patients and lots of trip to the radiologist, I became proficient in interpreting my own MRI films. Although an ineffective way to learn (formal training is much better), it opened my eyes on how to interpret MRI images, understand protocols and gave me an appreciation for the neuroradiologist.
The solution is obviously education and creating your own team. The time has long passed that the chiropractor needs to be part of the medical team. That notion is so long over, it should be dead! Each chiropractor needs to create their own team that includes the medical specialist, when needed. As a result, the clinical decision making is not abdicated to the MD, who has no training in chiropractic, and allows us to maintain full control of our patients using our team for input. Without the requisite training in understanding image protocols and the basics of reading images, we are left in the above paradigm that the survey results brought out and then are forced to be part of the medical specialist’s team, because we will not have the necessary knowledge, mandating someone else, usually the MD specialist, to make the tough decisions and dictate to us the care of our patients.
Does this mean we need to become radiologists? No, we need the knowledge and the credentials in reading MRI images and then we can utilize the radiologist as part of our team, to confirm what we are seeing. This brings us to the first member of our team, the radiologist, or more specifically, the neuroradiologist, who is a radiologist that spends an additional one to two years in training focused solely on brain and spine. I not only choose to be the best-of-the-best in clinical excellence through hard work; I also choose to only work with the best-of-the-best and the neuroradiologist is it.
As a note, once I started to interpret my own MRI’s, I had numerous disagreements with the general radiologist’s conclusions and, after bringing the neuroradiologist onto my team, I rarely had a disagreement.
The second member of my team is the neurosurgeon. If there is a space occupying lesion, such as a herniated disc on the cord or root, I confer with the neurosurgeon to ensure an accurate diagnosis, so I can make the clinical decision for my patient. There is no need for “gray areas” in disc-related diagnosis with today’s technology and your ability to assemble your team. This ensures an accurate prognosis and treatment plan.
Over time, the medical specialists will see you as their equal, based upon your clinical excellence and the feedback your patients are giving them in consultation. In the end, this will equate to increased referrals and help to eradicate any negative stigmas that some of the “medical fringe” still harbor towards chiropractic. When you are in conference with co-treating doctors, either primary care or specialists, and you know as much or more than they do, it is only a matter of time before they will be reaching out to you for the solution to their patient’s non-surgical spinal-related care.
This is how to build a referral network from the medical community. This is another example of how the only way to win for a lifetime is through clinical excellence. All it takes is a commitment to learn and the direction is clear. Once you have that level of knowledge with the understanding that the learning is ongoing, all that remains is how you communicate with your patients and community.
The message is simple; get the knowledge, the credentials, create your own team and be in control.
 Dr. Mark Studin is the President of CMCS Management which offers the Lawyers Marketing Program,Family/MD Marketing Program and Compliance Auditing services. He can be contacted at www.TeachChiros.com or call 1-631-786-4253
Dr. Mark Studin is the President of CMCS Management which offers the Lawyers Marketing Program,Family/MD Marketing Program and Compliance Auditing services. He can be contacted at www.TeachChiros.com or call 1-631-786-4253


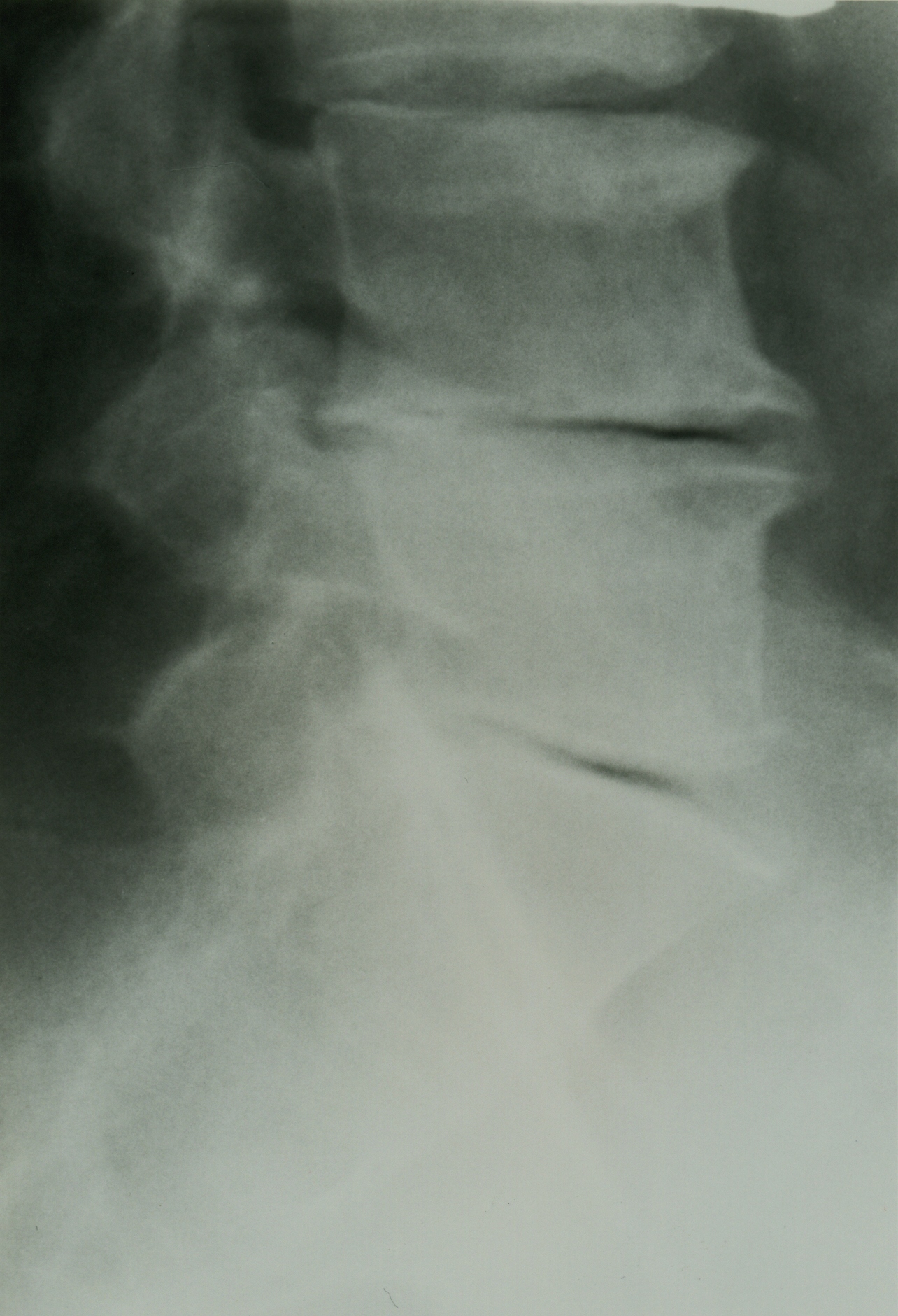




 Diagnosis: Kienbock’s Disease
Diagnosis: Kienbock’s Disease






 Dr. Mark Studin is the President of CMCS Management which offers the Lawyers Marketing Program,Family/MD Marketing Program and Compliance Auditing services. He can be contacted at
Dr. Mark Studin is the President of CMCS Management which offers the Lawyers Marketing Program,Family/MD Marketing Program and Compliance Auditing services. He can be contacted at