:dropcap_open:I:dropcap_close:s it possible to walk through a doorway when the door is closed? That strange question is a metaphor that can be used to describe the difference in research-based rehabilitation to prepare the spine for corrective procedures with little to no pain versus no preparation at all or, worse yet, substituting bilateral strengthening exercises for rehab to prepare the spine for corrections that are often both painful and ineffective.
:dropcap_open:I:dropcap_close:s it possible to walk through a doorway when the door is closed? That strange question is a metaphor that can be used to describe the difference in research-based rehabilitation to prepare the spine for corrective procedures with little to no pain versus no preparation at all or, worse yet, substituting bilateral strengthening exercises for rehab to prepare the spine for corrections that are often both painful and ineffective.
Gym type exercises are often called rehabilitation exercises. However, the two have little in common. Gym type exercises are isotonic that work and shorten muscles, thereby opposing positional changes. Phasic muscles are enervated by a1-motor fibers and are consciously controlled and, when totally fatigued or injured, become flaccid. Postural muscles are enervated by a2-motor fibers and are autonomic nerve controlled. The strengthening of these muscles requires isometric exercises. When they are fatigued or injured, they become spastic. It is critical to understand that postural muscles dominate one’s spinal position and function as well as posture, stance and gait.
What is rehabilitation and why is it necessary for quality patient care? Dorland’s Medical Dictionary 26th Ed. defines rehabilitation as:
1. “The restoration of normal form and function after injury or illness.”
2. “The restoration of an ill or injured patient to self-sufficiency or to gainful employment at the highest attainable skill in the shortest period of time”.
The profession of chiropractic claims that the adjustment is for the restoration of normal form and function of the spine through correction of spinal displacement subluxations. We can agree that abnormal/subluxated spinal forms cause abnormal functions.
Surveys show that the clinical procedures taught in chiropractic colleges and practiced by 84% of the profession involve the use of a sudden applied force into the subluxated spine, referred to as an adjustment or treatment.
What do the adjusting forces actually do? Is it possible to physically correct spinal displacement subluxations without first preparing the spine to welcome the force through rehabilitating the soft tissues that hold the static spine upright while in a normal or abnormal (subluxated) position?
:dropcap_open:We can agree that abnormal/subluxated spinal forms cause abnormal functions.:quoteleft_close:
Research published in 1996, by JMPT, titled “Lasting Changes in Passive Range of Motion after Spinal Mobilization,” a Randomized, Blind Controlled Trial, tested spinal changes produced by diversified and toggle recoil adjusting. Their findings were that these adjustments caused about a 5% increase in mobility and the changes lasted for about 7 days. A more recent article published in the Spine Journal demonstrated with pre and post MRI studies that the same kinds of adjusting resulted in the spine becoming measurably more displaced than before it was adjusted. Chiropractic adjusting, without first performing rehabilitation to prepare the spinal soft tissues for change, typically has shown little success in making gross structural spinal and postural changes. This also was tested and published in JMPT. The authors were Harrison, et al in 1997, and Lantz et al, in 2001. In 1975, Jowett and Fidler published research in Orthop. Clin., N. Amer. that proved the body changes phasic fibers into postural muscle fibers on the convex side of spinal displacement subluxations; hypo mobility and nerve root compression were also noted.
Neuro-muscular research has proven that the dynamic stretch reflex guards all body parts including spinal position, even if it is in a subluxated position from being changed by sudden applied forces. Guyton’s Physiology 5th and 6th Edition, explains how the dynamic stretch reflex causes muscles to replace body parts after a dynamic force has displaced them. Muscles intercept sudden applied forces of up to .3 of a second in speed. The phasic muscle fibers can contract fast enough to counteract these sudden applied forces. This reflex protection is automatic, unless the force is faster than .3 seconds or so great that they tear the muscles and then the ligaments, thereby causing spinal subluxations.
The protective energy of the muscles can be greatly reduced by slowly stretching the phasic and postural muscles rather than attempting to exercise them. To be effective, stretching should last at least 40 seconds and include all muscles involved.
:quoteright_open:Hysteresis can temporarily remove up to 95% of the ligament’s holding energy and lasts for approximately six minutes.:quoteright_close:
Ligament research has proven that to instantly change a vertebrae’s position, the adjusting force would have to overcome 40% of the ligament’s resisting force. Such high forces are impossible for a doctor to produce and could crush the vertebrae before the ligament entered the plastic range necessary, before instant positional change of a vertebra can occur. However, rehabilitation procedures that cause disks and ligaments to go through full range loading and unloading cycle’s for 2 to 5 minutes produces a condition called hysteresis, which gradually lowers the resistance of spinal disks and ligaments, thereby making changes in spinal position possible, easy and pain free. Hysteresis can temporarily remove up to 95% of the ligament’s holding energy and lasts for approximately six minutes after loading and unloading cycles are discontinued. Within 15 to 20 minutes after loading and unloading cycles are discontinued, the ligaments regain all of their holding energy.
Loading and unloading cycles in the cervical spine requires slow, intermittent traction, while effective loading and unloading cycles in the lumbo-sacral spine require full range, figure 8 cycles that are slowly applied, requiring 4 seconds to complete one cycle after the ligaments are completely stretched. The figure-8 cycles also mix and re-mix the protoglycine aggregate of the disk’s nucleus necessary for making and maintenance of a perfect jell. Like fluids, the jelled nucleus is non-compressible. When perfected, it equally transfers body weight from the vertebrae above to the vertebrae below, thereby providing a foundation for maintenance of the corrected spine’s form and function. In addition, the figure-8 motion pumps the cerebral-spinal fluids necessary for the metabolic interchange of glucose to feed the brain, thereby giving the patient a feeling of mental and physical well being—an additional benefit of the rehab procedures! Home care instructions work in tandem with clinical care and will include the use of deep, diaphragmatic breathing in coordination with specific rehabilitation procedures. These procedures take into account the fact that the thoracic spine is approximately 13 times less flexible than the cervical spine and approximately 3 times less flexible than the lumbar spine; therefore, thoracic loading and unloading cycles require more time and concerted rehabilitation procedures. Patients are taught to prepare their spine both in the clinic before being seen, as well as at home before daily activities and rest.
Change is inevitable for the growth of any profession; without it, stagnation and eventual decline is the end result. Through the use of clinical research and documentation with new and more efficient methodologies, we grow in our knowledge and our abilities. The Pettibon Biomechanics Institute has published several retrospective as well as blinded studies, proving through pre- and post- X-rays that permanent spinal corrections are possible after the spinal soft tissues have been prepared through our holistic rehabilitation procedures. Research can be found at www.pettiboninstitute.org.
Burl R. Pettibon, DC, FABCS, FRCCM, PhD. (Hon) has guided The Pettibon Institute’s direction, continuing education offerings, and research since the Institute’s inception as the Pettibon Spinal Bio-Mechanics Institute in 1981. As a teacher, inventor, and researcher, Dr. Pettibon’s influence and contributions to the science of chiropractic are legendary. Dr. Pettibon has been an extension faculty member and lecturer at Palmer College of Chiropractic for more than 35 years. He has also been an extension faculty member at Life University, Logan College of Chiropractic, Parker College of Chiropractic, and Cleveland Chiropractic College—where he received his degree in 1956. Dr. Pettibon has written more than 65 papers and books on chiropractic care and research. Over the course of his career, he has developed 25 clinics. At the present time, the profession is using the more than 50 rehabilitative products that he has invented to make the detection and correction of vertebral displacements both easier and more accurate. He currently holds four patents. Papers and books are also available through www.pettibonsystem.com.
References
1.Morningstar MW, Strauchman MN, Weeks DA, Spinal Manipulation and Anterior Headweighting for the Correction of Forward Head Posture and Cervical Hypolordosis: A Pilot Study, Spring 2003, Number 2, Volume 2, Journal of Chiropractic Medicine.
2.Horseman I, Morningstar MW, Radiographic disk height increase after a trial of multimodal spine rehabilitation and vibration traction: a retrospective case series, 2008 7, 140-145, Journal of Chiropractic Medicine, 2008.
3.Schwab MJ, Chiropractic management of a 47-year-old firefighter with lumbar disk extrusion, 7, 146-154, Journal of Chiropractic Medicine, 2008.
4.Saunders ES, Woggon E, Cohen C, Robinson DH, Improvement of Cervical Lordosis and Reduction of Forward Head Posture with Anterior Head Weighting and Proprioceptive Balancing Protocols, J. Vertebral Subluxation Res., April 27, 2003.
5.Morningstar MW, Cervical curve restoration and forward head posture reduction for the treatment of Mechanical thoracic pain using the Pettibon corrective and rehabilitative procedures, Summer 2002, Number 3, Volume 1, Journal of Chiropractic Medicine.
6.Morningstar MW, Cervical hyperlordosis, forward head posture, and lumbar Kyphosis correction: a novel treatment for Mid-thoracic pain, Spring 2003, Number 3, Volume 2, Journal of Chiropractic Medicine.


 Now that genetic pre-disposition testing for scoliosis progression risk is available, An Early Stage Intervention Program has also been developed to provide scoliosis patients a non-bracing, non-surgical treatment option that allows them to take immediate action in the prevention of the next stage of the standard treatment process.
Now that genetic pre-disposition testing for scoliosis progression risk is available, An Early Stage Intervention Program has also been developed to provide scoliosis patients a non-bracing, non-surgical treatment option that allows them to take immediate action in the prevention of the next stage of the standard treatment process.



 As if all this wasn’t enough, other forces come into play to create a low back that is less stable and more prone to create chronic pain and discomfort. Shear forces to be exact. In a person with normal posture, downward Gravitational and directional shear forces work with the body to “lock” joints into position under load, thereby providing strength and stability to the spine. In a pregnancy posture, the Gravitational forces remain essentially the same, but the shear forces change direction in such a way as to open the low back joints, providing less stability in the spine. The body’s exquisite feedback system senses this and the muscles in the low back become tighter in an effort to take up the slack.
As if all this wasn’t enough, other forces come into play to create a low back that is less stable and more prone to create chronic pain and discomfort. Shear forces to be exact. In a person with normal posture, downward Gravitational and directional shear forces work with the body to “lock” joints into position under load, thereby providing strength and stability to the spine. In a pregnancy posture, the Gravitational forces remain essentially the same, but the shear forces change direction in such a way as to open the low back joints, providing less stability in the spine. The body’s exquisite feedback system senses this and the muscles in the low back become tighter in an effort to take up the slack.
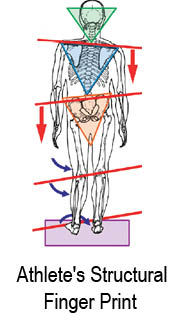
 which will exhibit “Short Weakness”. With that knowledge, a Posture Reprogramming professional can create an exercise program to strengthen the muscles that have become stretched, and a stretching program for the muscles that have become shotened.
which will exhibit “Short Weakness”. With that knowledge, a Posture Reprogramming professional can create an exercise program to strengthen the muscles that have become stretched, and a stretching program for the muscles that have become shotened.
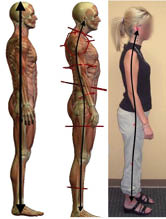

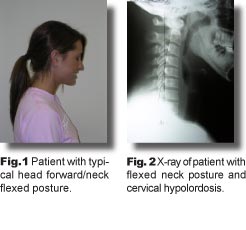
 The most common abnormal posture profile is illustrated on the right. The head sits forward of the shoulders, the upper back has drifted backward and the pelvis has tipped forward. This is commonly known as Forward Head Posture (FHP). Notice the straight plumb line we expect to see in good posture now has a substantial curve in FHP. It’s been estimated that 80% of the general population has varying degrees of FHP.
The most common abnormal posture profile is illustrated on the right. The head sits forward of the shoulders, the upper back has drifted backward and the pelvis has tipped forward. This is commonly known as Forward Head Posture (FHP). Notice the straight plumb line we expect to see in good posture now has a substantial curve in FHP. It’s been estimated that 80% of the general population has varying degrees of FHP.
 32 years ago, when just starting in practice, I contacted our local high school football coach and offered my services to his team. A couple times a week I would work on any players who asked for help. As great as the job seemed, it was short lived. As soon as the school physician got wind of my involvement, I was introduced to the politics of sports. The athletic director informed me I was not to come onto the campus again.
32 years ago, when just starting in practice, I contacted our local high school football coach and offered my services to his team. A couple times a week I would work on any players who asked for help. As great as the job seemed, it was short lived. As soon as the school physician got wind of my involvement, I was introduced to the politics of sports. The athletic director informed me I was not to come onto the campus again. When an athlete becomes injured, the goal is to reduce the symptoms, but never correct the underlying problem. Fig. 1 shows an example of the biomechanical imbalances that exist in all of us, and it is these imbalances that lead to the majority of injuries in athletes. These imbalances originate in the feet (our foundation) and if this imbalance is not addressed, we have a limited potential in balancing the rest of the structure.
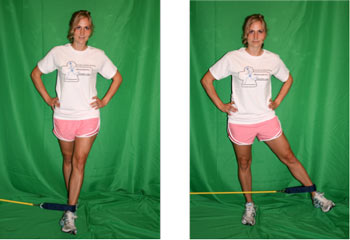
When an athlete becomes injured, the goal is to reduce the symptoms, but never correct the underlying problem. Fig. 1 shows an example of the biomechanical imbalances that exist in all of us, and it is these imbalances that lead to the majority of injuries in athletes. These imbalances originate in the feet (our foundation) and if this imbalance is not addressed, we have a limited potential in balancing the rest of the structure.
 :dropcap_open:B:dropcap_close:ack injuries in adolescents are not very common, but add participation in athletics and you increase the opportunity of experiencing some form of low back pain. According to Micheli, back injuries of young athletes are a significant phenomenon, estimated to occur in 10 to 15 percent of participants1. The prevalence will vary, based on certain sports. In sports like gymnastics back injuries are 11 percent whereas, in football linemen, it has been recorded as high as 50 percent2.
:dropcap_open:B:dropcap_close:ack injuries in adolescents are not very common, but add participation in athletics and you increase the opportunity of experiencing some form of low back pain. According to Micheli, back injuries of young athletes are a significant phenomenon, estimated to occur in 10 to 15 percent of participants1. The prevalence will vary, based on certain sports. In sports like gymnastics back injuries are 11 percent whereas, in football linemen, it has been recorded as high as 50 percent2.