KEY POINTS FROM DR. DAN MURPHY
1) The results of this study are “the most comprehensive and comparable quantitative assessment of the mortality burden of important modifiable risk factors in the US population, and the only one to include the effects of multiple dietary and metabolic factors.”
2) “A number of modifiable factors are responsible for many premature or preventable deaths. For example, being overweight or obese shortens life expectancy, while half of all long-term tobacco smokers in Western populations will die prematurely from a disease directly related to smoking.”
3) “Of the 2.5 million US deaths in 2005, they estimate that nearly half a million were associated with tobacco smoking and about 400,000 were associated with high blood pressure.” These two risk factors, therefore, each accounted for about 1 in 5 deaths in US adults.
4) “Overweight, obesity and physical inactivity were each responsible for nearly 1 in 10 deaths.”
5) “Among the dietary factors examined, high dietary salt intake had the largest effect, being responsible for 4% of deaths in adults.”
6) Findings: US deaths from risk factors, 2005
| Tobacco smoking |
467,000 |
| High blood pressure |
395,000 |
| Overweight–obesity |
216,000 |
| Physical inactivity |
191,000 |
| High dietary salt |
102,000 |
| Low dietary omega-3 fatty acids |
84,000 |
| High dietary trans fatty acids |
82,000 |
| Alcohol use |
64,000 |
Although 26,000 deaths from ischemic heart disease, ischemic stroke, and diabetes were averted by current alcohol use, they were outweighed by 90,000 deaths from other cardiovascular diseases, cancers, liver cirrhosis, pancreatitis, alcohol use disorders, road traffic and other injuries, and violence.
7) “The mortality-reducing effects of omega-3 fatty acids and of replacing saturated fatty acids (SFA) with polyunsaturated fatty acids (PUFA) have been confirmed in randomized trials.” [IMPORTANT]
8) In the year 2005, 2,448,017 US residents died.
A)) 96% percent of all deaths in the US were in people ≥30 yrs. of age.
9) The four most common causes of death were:
| Ischemic heart disease |
434,000 deaths |
| Lung cancer |
163,000 deaths |
| Stroke |
150,000 deaths |
| Chronic obstructive pulmonary diseases |
124,000 deaths |
10) “The single largest risk factor for cardiovascular mortality in the US was high blood pressure, responsible for an estimated 395,000 cardiovascular deaths (45% of all cardiovascular deaths), followed by overweight–obesity, physical inactivity, high LDL cholesterol, smoking, high dietary salt, high dietary trans fatty acids, and low dietary omega-3 fatty acids.”
11) “Smoking had the largest effect on cancer mortality compared with any other risk factor, causing an estimated 190,000 (184,000–194,000) or 33% of all cancer deaths.”
12) “40% or more of all deaths attributable to high LDL cholesterol, overweight–obesity, high dietary trans fatty acids, low dietary PUFA and omega-3 fatty acids, low intake of fruits and vegetables, alcohol use, and smoking occurred before 70 years of age.”
13) “Smoking was by far the leading cause of death in both men and women ≤70 years, followed by overweight–obesity.”
14) “29% of the chronic disease mortality effects of alcohol use occurred among heavy drinkers (i.e., men who consumed more than 60 grams of pure alcohol or 4 drinks per day and women who consumed more than 40 grams per day); this group did not have any mortality benefits from alcohol use. In contrast, in those who had light alcohol consumption (up to 40 g per day for men and 20 g per day for women), the protective effects on ischemic heart disease and diabetes mortality were larger than the hazardous effects from other chronic diseases, leading to an overall reduction in mortality in this group.”
[As long as one does not drink and drive a vehicle, 2 alcoholic drinks per day for men and 1 alcoholic drink per day for women reduces their chance of death; however, any more than that and alcohol increases death.]
15) “If the entire adult US population had light alcohol consumption, a total of 12,000 cardiovascular deaths would be prevented, largely among adults aged ≥45 y. However, this level of alcohol consumption would also cause an estimated 8,000 deaths due to road traffic accidents, largely among adults aged <30 y.”
16) One hour of vigorous physical activity per day would prevent 62,000 deaths per year compared to doing only 20 min of moderate activity every day.
17) “The results of our analysis of dietary, lifestyle, and metabolic risk factors show that targeting a handful of risk factors has large potential to reduce mortality in the US, substantially more than the currently estimated 18,000 deaths averted annually by providing universal health insurance.”
COMMENTS FROM DR. DAN MURPHY:
In light of current discussion concerning universal health insurance, this article notes that vigorous exercise would save 3.4 times the lives (62,000) as would universal health insurance coverage (18,000).
High blood pressure is a significant problem in America. This underscores the importance of the results of the 2007 article by Marshall Dickholtz, D.C:
G. Bakris, M. Dickholtz Sr., P. M. Meyer, G. Kravitz, E. Avery, M. Miller, J. Brown, C. Woodfield and B. Bell. Atlas vertebra realignment and achievement of arterial pressure goal in hypertensive patients: a pilot study. Journal of Human Hypertension. March 2, 2007.
 Dr. Dan Murphy graduated magna cum laude from Western States Chiropractic College in 1978. He received Diplomat status in Chiropractic Orthopedics in 1986. Since 1982, Dr. Murphy has served part-time as undergraduate faculty at Life Chiropractic College West, currently teaching classes to seniors in the management of spinal disorders. He has taught more than 2000 postgraduate continuing education seminars. Dr. Murphy is a contributing author to both editions of the book Motor Vehicle Collision Injuries and to the book Pediatric Chiropractic. Hundreds of detailed Article Reviews, pertinent to chiropractors and their patients, are available at Dr. Murphy’s web page, www.danmurphydc.com. TAC
Dr. Dan Murphy graduated magna cum laude from Western States Chiropractic College in 1978. He received Diplomat status in Chiropractic Orthopedics in 1986. Since 1982, Dr. Murphy has served part-time as undergraduate faculty at Life Chiropractic College West, currently teaching classes to seniors in the management of spinal disorders. He has taught more than 2000 postgraduate continuing education seminars. Dr. Murphy is a contributing author to both editions of the book Motor Vehicle Collision Injuries and to the book Pediatric Chiropractic. Hundreds of detailed Article Reviews, pertinent to chiropractors and their patients, are available at Dr. Murphy’s web page, www.danmurphydc.com. TAC





 Dr. Dan Murphy graduated magna cum laude from Western States Chiropractic College in 1978. He received Diplomat status in Chiropractic Orthopedics in 1986. Since 1982, Dr. Murphy has served part-time as undergraduate faculty at Life Chiropractic College West, currently teaching classes to seniors in the management of spinal disorders. He has taught more than 2000 postgraduate continuing education seminars. Dr. Murphy is a contributing author to both editions of the book Motor Vehicle Collision Injuries and to the book Pediatric Chiropractic. Hundreds of detailed Article Reviews, pertinent to chiropractors and their patients, are available at Dr. Murphy’s web page,
Dr. Dan Murphy graduated magna cum laude from Western States Chiropractic College in 1978. He received Diplomat status in Chiropractic Orthopedics in 1986. Since 1982, Dr. Murphy has served part-time as undergraduate faculty at Life Chiropractic College West, currently teaching classes to seniors in the management of spinal disorders. He has taught more than 2000 postgraduate continuing education seminars. Dr. Murphy is a contributing author to both editions of the book Motor Vehicle Collision Injuries and to the book Pediatric Chiropractic. Hundreds of detailed Article Reviews, pertinent to chiropractors and their patients, are available at Dr. Murphy’s web page, 

 In each issue, a clinical topic will be covered by Dr. William J. Owens of the American Academy of Medical Legal Professionals (AAMLP), which is a national, non-profit organization, comprised of doctors and lawyers. The purpose of the organization is to provide its members with current research in trauma and spinal related topics, to keep the profession on the cutting edge of healthcare. Members may also sit for a Diplomate examination and be conferred a DAAMLP. The organization also offers support to the individual member’s practice. To learn more, go to
In each issue, a clinical topic will be covered by Dr. William J. Owens of the American Academy of Medical Legal Professionals (AAMLP), which is a national, non-profit organization, comprised of doctors and lawyers. The purpose of the organization is to provide its members with current research in trauma and spinal related topics, to keep the profession on the cutting edge of healthcare. Members may also sit for a Diplomate examination and be conferred a DAAMLP. The organization also offers support to the individual member’s practice. To learn more, go to 
 Dr. Dan Murphy graduated magna cum laude from Western States Chiropractic College in 1978. He received Diplomat status in Chiropractic Orthopedics in 1986. Since 1982, Dr. Murphy has served part-time as undergraduate faculty at Life Chiropractic College West, currently teaching classes to seniors in the management of spinal disorders. He has taught more than 2000 postgraduate continuing education seminars. Dr. Murphy is a contributing author to both editions of the book Motor Vehicle Collision Injuries and to the book Pediatric Chiropractic
Dr. Dan Murphy graduated magna cum laude from Western States Chiropractic College in 1978. He received Diplomat status in Chiropractic Orthopedics in 1986. Since 1982, Dr. Murphy has served part-time as undergraduate faculty at Life Chiropractic College West, currently teaching classes to seniors in the management of spinal disorders. He has taught more than 2000 postgraduate continuing education seminars. Dr. Murphy is a contributing author to both editions of the book Motor Vehicle Collision Injuries and to the book Pediatric Chiropractic
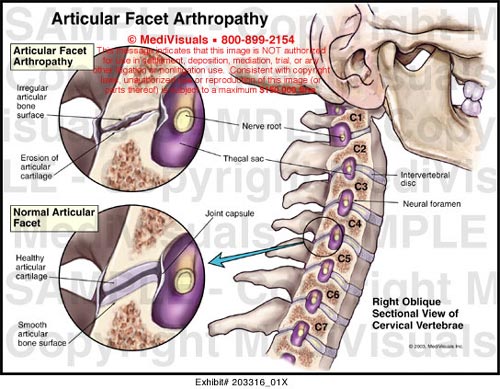
 When evaluating a patient that was traumatically injured, there are two important aspects to consider. The first is rendering an accurate diagnosis and the second is clearing the patient to administer the chiropractic adjustment. Both are important to the patient’s health, your license and your reputation as a doctor. In an important article published some time ago in Spine, the authors took a look at the effects of a narrowed central canal pre-disposing a trauma victim to further neurological injury. In other words, would a patient with congenital or spondylitic stenosis of the central canal be susceptible to worse injury when compared to a healthy control?
When evaluating a patient that was traumatically injured, there are two important aspects to consider. The first is rendering an accurate diagnosis and the second is clearing the patient to administer the chiropractic adjustment. Both are important to the patient’s health, your license and your reputation as a doctor. In an important article published some time ago in Spine, the authors took a look at the effects of a narrowed central canal pre-disposing a trauma victim to further neurological injury. In other words, would a patient with congenital or spondylitic stenosis of the central canal be susceptible to worse injury when compared to a healthy control?
 In each issue, a clinical topic will be covered by Dr. William J. Owens of the American Academy of Medical Legal Professionals (AAMLP), which is a national, non-profit organization, comprised of doctors and lawyers. The purpose of the organization is to provide its members with current research in trauma and spinal related topics, to keep the profession on the cutting edge of healthcare. Members may also sit for a Diplomate examination and be conferred a DAAMLP. The organization also offers support to the individual member’s practice. To learn more, go to
In each issue, a clinical topic will be covered by Dr. William J. Owens of the American Academy of Medical Legal Professionals (AAMLP), which is a national, non-profit organization, comprised of doctors and lawyers. The purpose of the organization is to provide its members with current research in trauma and spinal related topics, to keep the profession on the cutting edge of healthcare. Members may also sit for a Diplomate examination and be conferred a DAAMLP. The organization also offers support to the individual member’s practice. To learn more, go to