Journal of Bone and Joint Surgery (American)
Journal of Bone and Joint Surgery (American)
April 1947, Vol. 29, No. 2, pp. 461-534
Verne T. Inman and John B. de C. M. Saunders
1) “Herniation of the nucleus pulposus or protrusion of the disc is now firmly established as a pathological mechanism associated with low-back pain and sciatica.”
2) “The majority will agree that the treatment of many of these cases by laminectomy and nerve-root decompression has been disappointing.”
3) “Destroy the disc and you destroy spinal mechanics. Therefore, in disc derangement, we are dealing with a dual problem:”
A) Deranged spinal mechanics
B) The effects of spinal nerve-root irritation and compression
[Spinal nerve root irritation and compression are often very different physiologically. Compression reduces nerve function and, hence, is associated with things such as muscle atrophy and reduced sensation. Irritation increases (denervation supersensitivity {Gunn}) nerve function and, hence, is associated with things such as increased pain, increased muscle tone and spasm.]
4) Both “deranged spinal mechanics,” nerve root irritation, and nerve root compression, cause pain.
5) Patients with deranged spinal mechanics” should not be surgically managed. [“Deranged spinal mechanics” appears to be synonymous with chiropractic subluxation.]
6) The normal nucleus pulposus is a semifluid substance, being 80% water and, thus, is “incompressible.”
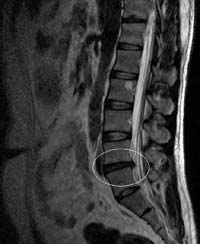
7) The normal semifluid nucleus transmits forces to the elastic spinal ligamentous structures. “The critical feature in the disturbance of spinal mechanics and in the production of pain is the effect on the ligamentous structures, caused by the loss of water or nuclear substance following injury or degeneration.” [Key Point]
8) “An individual getting up in the morning is taller than when he [she] goes to bed at night:” men by ¾ inch, women by ½ inch. This is because the nucleus loses fluid in an upright gravity environment. This exchange of fluid helps the nucleus and annulus of the disc to remain healthy.
9) With age, the cartilaginous end-plate becomes less permeable to fluid, the free exchange of water is suppressed, resulting in “progressive desiccation of the nucleus.”
10) Small rents in the annulus allow the nucleus to escape, reducing fluid pressure and altering spinal mechanics, and pain.
[Sounds like Gonstead’s internal disc derangement.]
11) The resiliency of the spine and the motions permitted to it are primarily due to the elastic nature of the annulus fibrosis.
12) “The loss of the fluid pressure in the nucleus pulposus leads to grave derangements in the physiology of the disc.”
13) “The decrease in the vertical height of the intervertebral disc spaces leads to subluxation of the interarticular zygapophysial joints, in which degenerative changes develop as the result of the abnormal forces acting upon them.” [Subluxation]
14) “The ligamentous structures of the body are the most sensitive to pain.”
15) Ligaments can initiate pain from chemical irritants or from “mechanical displacement of the collagenous fibers.” This pain is deep, dull aching and poorly localized. [Chiropractic Subluxation]
16) Ligament pain ebbs and wanes, and can be accompanied by “vasovagal responses, such as nausea, sweating, and fall in blood pressure.”
17) Deep ligament pain arises embryologically from the mesoderm. This type of pain is termed “sclerotogenous” pain, meaning it does not follow a dermatomal distribution.
18) Deep sclerotogenous pain can occur in the absence of direct irritation of the peripheral nerve or nerve root.
19) “The annulus fibrosus has been shown to possess a rich nerve supply,” allowing it to initiate “sclerotogenous” pain.
20) Distortion of the annulus and other spinal ligaments can cause not only local pain, but also sclerotomal pain that radiates down the posterior thigh. This is not sciatica, because there is no irritation to the nerve roots.
21) When the lumbar nerve roots exit the intervertebral foramen, they carry with it the spinal dura, doubling their diameter as compared to the cauda equina roots in the subarachnoid space.
22) Since each nerve root is firmly attached to the spinal dura, “traction upon the nerve will produce deformation of the dural sac without transmission of the tension to the fibers of the cauda equina.”
23) Deeper spinal structures primarily initiate slow pain, which is characterized as being dull and aching, and poorly localized.
24) Nerve compression primarily affects large nerve fibers, which are associated with proprioceptive and motor function.
25) Pain fibers are smaller, and are more likely to fire in response to chemical (inflammatory) stimulus than to mechanical pressure.
26) Disc herniation without nerve compression is characterized first by pain and then a deep ache radiating into the leg in a sclerotomal pattern.
27) Disc herniation with nerve compression is characterized by loss of vibratory sense, muscle weakness, reduced tendon reflexes, and hyperesthesia/pain in a dermatomal pattern. The pain is sharper from chemical inflammation in the region.
28) This all indicates that patients can be placed into three categories:
A)) Mechanical spinal derangement: [chiropractic subluxation]
These patients have deep spinal irritations but no nerve compression.
These patients have “backache and local signs and symptoms of injury to the vertebral ligamentous structures, have radiating pain, deeper in character, extending down one or both extremities. The extent of the radiation is indicative in some measure of the degree of irritation or injury to the ligamentous structures.”
B)) Nerve root compression from disc herniation:
The “pressure will interrupt nerve conductivity in a precise sequential fashion:”
The larger nerve fibers conveying proprioception and motor impulses are affected first.
The nerve fibers conveying pressure, touch and fast pain are affected second.
The nerve fibers conveying temperature sense and deep pain are lost last.
These patients usually also have spinal ligamentous irritation that causes local backache and the “radiation of deep pain to the extremities.” Surgery to decompress the nerve root will often leave the patient with the ligamentous back pain and deep extremity referred pain radiation, and the patient will often be disappointed.
C)) Nerve root compression from spinal cord tumor:
The major lesion is nerve compression, but local ligamentous irritation is minimum or lacking. There are outstanding signs of nerve compression, including muscle weakness with atrophy, “definite and unequivocal loss of sensation over the appropriate dermatome, and reflex changes.” Backache is mild or lacking. Radiation of pain to the lower extremity is not extensive. This is typically caused by a spinal cord tumor, and only rarely from a disc herniation. Surgical removal and decompression of the nerve usually results in complete and dramatic recovery.
DISCUSSION BY WILLIAM JASON MIXTER:
29) “Motor weakness should be considered a definite emergency and the patient should be operated upon at once. If the motor weakness is left untreated for a considerable time [6-12 months], the strength never returns.”
DISCUSSION BY BARNES WOODHALL:
30) 40% of disc herniation patients with nerve compression have only motor signs, they “possessed no defecit in the common sensory modalities of pain, light touch, heat and cold, or sense of position.”
Dr. Dan Murphy graduated magna cum laude from Western States Chiropractic College in 1978. He received Diplomat status in Chiropractic Orthopedics in 1986. Since 1982, Dr. Murphy has served part-time as undergraduate faculty at Life Chiropractic College West, currently teaching classes to seniors in the management of spinal disorders. He has taught more than 2000 postgraduate continuing education seminars. Dr. Murphy is a contributing author to both editions of the book Motor Vehicle Collision Injuries and to the book Pediatric Chiropractic. Hundreds of detailed Article Reviews, pertinent to chiropractors and their patients, are available at Dr. Murphy’s web page, www.danmurphydc.com.