
Molecular Neurobiology
January 29, 2011 [epub]
Artemis P. Simopoulos
This article has 116 references
LA = linoleic acid (plant derived omega-6 fatty acid)
ALA = alpha linolenic acid (plant derived omega-3 fatty acid)
Abstract
Several sources of information suggest that human beings evolved on a diet that had a ratio of omega-6 to omega-3 fatty acids (FA) of about 1/1. Today, Western diets have a ratio of 10/1 to 20–25/1, indicating that Western diets are deficient in omega-3 FA compared with the diet on which humans evolved and their genetic patterns were established. Omega-6 and omega-3 FA are not interconvertible in the human body and are important components of practically all cell membranes.
Studies with nonhuman primates and human newborns indicate that docosahexaenoic acid (DHA) is essential for the normal functional development of the brain and retina, particularly in premature infants. DHA accounts for 40% of the membrane phospholipid FA in the brain. Both eicosapentaenoic acid (EPA) and DHA have an effect on membrane receptor function and even neurotransmitter generation and metabolism.
There is growing evidence that EPA and DHA could play a role in hostility and violence in addition to the creating beneficial effects on substance abuse disorders and alcoholism. The balance of omega-6 and omega-3 FA is important for homeostasis and normal development throughout the life cycle.
KEY POINTS FROM THIS STUDY:
1) Nutrition is an environmental factor that influences gene expression.
2) Major changes have taken place in our diet over the past 10,000 years since the beginning of the Agricultural Revolution, but our genes have not changed.
3) “Our genes today are very similar to the genes of our ancestors during the Paleolithic period 40,000 years ago, at which time our genetic profile was established.”
4) “Humans today live in a nutritional environment that differs from that for which our genetic constitution was selected.”
5) The major changes that have taken place in our diets in the past 10,000 years include:
A) An increase in energy intake and decrease in energy expenditure

B) An increase in saturated fat
C) An increase in omega-6 fatty acids
D) An increase in trans-fatty acids
E) An increase in cereal grains
F) An increase in fruit and vegetable intake
G) A decrease in omega-3 fatty acid intake
H) A decrease in complex carbohydrate intake
I) A decrease in fiber intake
J) A decrease in protein
K) A decrease in antioxidants
L) A decrease in vitamin D
M) A decrease in calcium intake
6) “The increase in trans-fatty acids is detrimental to health.”
7) “The beneficial health effects of omega-3 fatty acids, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) were described first in the Greenland Eskimos who consumed a high seafood diet and had low rates of coronary heart disease, asthma, type 1 diabetes mellitus, and multiple sclerosis. Since that observation, the beneficial health effects of omega-3 fatty acids have been extended to include benefits related to cancer, inflammatory bowel disease, rheumatoid arthritis, psoriasis, and mental health.”
8) The change of omega-6/omega-3 ratio in the food supply of Western societies has occurred over the last 150 years.
9) “During evolution, omega-3 fatty acids were found in all foods consumed: meat, wild plants, eggs, fish, nuts, and berries.”
10) Today in Western societies the omega-6/omega-3 ratio is very high due to the high intake of soybean, corn, sunflower, safflower, and linseed oils.
11) “LA is found in high amounts in grains with the exception of flaxseed, chia, perilla, rapeseed, and walnuts that are rich in ALA.”
12) The green leaves of plants are higher in ALA than LA.
13) The conversion of LA to EPA and DHA “appears to be limited and variable.”
14) The omega-6/omega-3 ratio is associated with normal “growth and development, as well as in the outcome of hypertension, cancer, arthritis, mental health, allergies and other autoimmune diseases,” as well as the “pathophysiology of atherosclerosis, inflammation, and aging.”
15) “DHA is found in high amounts in the membranes of the brain and retina and is critical for proper neurogenesis, neurotransmitter metabolism, neuroprotection and vision. The consumption of high amounts of DHA has been associated with multiple health benefits, including brain and retinal development, aging, memory formation, synaptic membrane function, photoreceptor biogenesis and function, and neuroprotection. DHA is essential for pre-natal brain development.”
16) Powerful anti-inflammatory molecules are derived from omega-3 fatty acids: Lipoxins, Resolvins, Protectins and Neuroprotectins. These molecules “function in the resolution of inflammation by activating specific mechanisms to promote homeostasis.”
:quoteright_open:The omega-6/omega-3 fatty acid ratio is innately critical for brain function, heart health, immunity, joint health, pain syndromes and more.:quoteright_close:
17) Omega-3s cause apoptotic death in cancer cells whereas omega-6s allowed the cancer cells to continue to proliferate.
18)Psychological stress in humans causes an overproduction of pro-inflammatory Cytokines, which are minimized with adequate levels of omega-3s.
19)Diets with a high omega-6/omega-3 ratio may enhance the risk for both depression and inflammatory diseases.
20) “LA more than any other nutrient is associated with shorter telomeres and shorter telomeres are associated with aging, cancer and coronary heart disease.”
21)“Clinical studies show that cognitive performance improves with omega-3s.”
22) “Positive effects of omega-3s on dementia, schizophrenia, and other central nervous system diseases have been reported.”
23) Omega-3s can affect not only cognitive functions, but also mood and emotional states and may act as a mood stabilizer. Omega-3s have beneficial effects in some neurological diseases in addition to chronic fatigue syndrome.
24) Omega-3 deficiency in childhood delays brain development and produces irreversible effects, while the same deficiency in aging accelerates the deterioration of brain function.
25) Omega-3 intake from ALA does not provide adequate intakes of EPA and DHA.
26) Substance abusers have low omega-3 fatty acid intakes due to poor dietary habits. Omega-3s are helpful in the treatment of cocaine dependence and alcoholism because they can stabilize neuron membranes.
27) Daily administration of 3 g of omega-3s for 3 months significantly decreased feelings of anger, anxiety and aggression.
28) “Western diets are characterized by high omega-6 and low omega-3 fatty acid intake, whereas during the Paleolithic period when human’s genetic profile was established, there was a balance between omega-6 and omega-3 fatty acids. Therefore, humans today live in a nutritional environment that differs from that for which our genetic constitution was selected.”
29) “The balance of omega-6/omega-3 fatty acids is an important determinant in maintaining homeostasis, normal development, and mental health throughout the life cycle.”
30) “It is known that the relative amounts of omega-6 and omega-3 in the cell membrane are responsible for affecting cellular function as the AA competes directly with EPA for incorporation into cell membranes.”
31) “A low AA/EPA ratio has been proposed as an index of the beneficial effects of omega-3s which have been shown in animal and clinical experiments.”
32) The balance of omega-3 and omega-6 fatty acids to the “developing brain may be necessary for normal growth and functional development.”
33) Omega-3 deficiency in the brain is associated with “decreased learning ability, with a lower synaptic vesicle density in the hippocampus; whereas, chronic administration of omega-3s improves reference memory-related learning probably due to increased neuroplasticity of the neural membranes.”
34) “Cognitive performance improves with omega-3’s supplementation, possibly due to increased hippocampal acetylcholine levels, the anti-inflammatory effects of omega-3s, decreased risk of cardiovascular disease or increased neuroplasticity.”
35) Omega-3 fatty acids have positive effects in patients with dementia, schizophrenia, depression and other central nervous systems diseases.
36) Omega-3 fatty acid supplementation could play a role in [reduced] hostility and violence.
37) “In carrying out clinical intervention trials, it is essential to increase the omega-3 and decrease the omega-6 fatty acid intake in order to have a balanced omega-6 to omega-3 intake.”
38) “In humans, the brain is the most outstanding organ in biological development: it follows that the priority is brain growth and development, and in the brain the balance between omega-6 and omega-3 PUFA metabolites is close to 1:1. This ratio should be the target for human nutrition.”
39) “In Western diets, the omega-6/omega-3 ratio has increased to between 10:1 and 20:1. This high omega-6 proportion is largely made up by LA, is far from optimal and is highly inappropriate for normal growth and development.”
40) “The ratio of omega-6/omega-3 fatty acids in the brain between 1:1 and 2:1 is in agreement with the data from the evolutionary aspects of diet and genetics.”
41) “A ratio of 1:1 to 2:1 omega-6/omega-3 fatty acids should be the target ratio for health.”
The omega-6/omega-3 fatty acid ratio is innately critical for brain function, heart health, immunity, joint health, pain syndromes and more. I believe that everyone should have the AA/EPA ratio tested to see if they are in the “target ratio” of 1-2/1, AA/EPA.
The lab we use to test the AA/EPA ratio is Metametrix, at (800) 221-4640.
The test is called Bloodspot Fatty Acids 0241.
The test is a finger prick draw, not venipuncture.
The omega-3 oils I take are from Nutri-West; I believe their ratios of ALA, EPA, DHA, and GLA are optimal: (800) 443-3333.
Nutri-West has a children’s formula, and both capsules and a liquid for adults:
CompleteChildren’s EPA/DHA (8 per day)
CompleteOmega-3 Essentials (6 per day), or
CompleteHi-Potency Omega-3 Liquid (1 teaspoon per day) for adults
To achieve the “target ratio” most adults need to consume 3,000 mg/d of EPA+DHA.
Dr. Dan Murphy graduated magna cum laude from Western States Chiropractic College in 1978. He received Diplomat status in Chiropractic Orthopedics in 1986. Since 1982, Dr. Murphy has served part-time as undergraduate faculty at Life Chiropractic College West, currently teaching classes to seniors in the management of spinal disorders. He has taught more than 2000 postgraduate continuing education seminars. Dr. Murphy is a contributing author to both editions of the book Motor Vehicle Collision Injuries and to the book Pediatric Chiropractic. Hundreds of detailed Article Reviews, pertinent to chiropractors and their patients, are available at Dr. Murphy’s web page, www.danmurphydc.com.
 Though chiropractic procedures have an enviable safety record, some studies have associated the risk of cerebral vascular incidents (stroke) with neck rotation and manipulation. This incidence has been estimated at 1 in 300,000 to 1 in 5.85 million manipulations, with some studies showing no causal relationship. No study has examined the incidence of adverse reactions following upper cervical spinal adjustments and the associated clinical outcomes. The Eriksen study is the first to clearly document the safety of multiple upper cervical techniques with a population of 1,090 patients receiving 2,653 upper cervical adjustments over an average of 17 days. Eighty-three doctors in four countries participated in this exclusively upper cervical study with Orthospinology, Grostic Procedure, NUCCA, Atlas Orthogonal, Advanced Atlas Orthogonal, Blair, Knee Chest, Duff, Toggle and SONAR techniques represented. Each doctor documented the response to care for 10 consecutive new patients for the two week period, with subjects ranging from 18 to 85 years of age with the mean age being 46.1 years. Females outnumbered males 699 (64.1%) to 391 (35.9%) and 95% of patients studied presented with headaches or musculoskeletal pain. No adjunct procedures such as full spine manipulation, mobilization, physical therapy or massage were utilized by the participating doctors, in order to maintain this study as purely upper cervical.
Though chiropractic procedures have an enviable safety record, some studies have associated the risk of cerebral vascular incidents (stroke) with neck rotation and manipulation. This incidence has been estimated at 1 in 300,000 to 1 in 5.85 million manipulations, with some studies showing no causal relationship. No study has examined the incidence of adverse reactions following upper cervical spinal adjustments and the associated clinical outcomes. The Eriksen study is the first to clearly document the safety of multiple upper cervical techniques with a population of 1,090 patients receiving 2,653 upper cervical adjustments over an average of 17 days. Eighty-three doctors in four countries participated in this exclusively upper cervical study with Orthospinology, Grostic Procedure, NUCCA, Atlas Orthogonal, Advanced Atlas Orthogonal, Blair, Knee Chest, Duff, Toggle and SONAR techniques represented. Each doctor documented the response to care for 10 consecutive new patients for the two week period, with subjects ranging from 18 to 85 years of age with the mean age being 46.1 years. Females outnumbered males 699 (64.1%) to 391 (35.9%) and 95% of patients studied presented with headaches or musculoskeletal pain. No adjunct procedures such as full spine manipulation, mobilization, physical therapy or massage were utilized by the participating doctors, in order to maintain this study as purely upper cervical.


 Artemis P. Simopoulos
Artemis P. Simopoulos
 As mentioned, low back pain is one of the most common conditions encountered in clinical practice and medications are the most commonly used type of treatment, and muscle relaxers are a common drug that has been prescribed by medical doctors for years for nonspecific low back pain, according to Chou (2010). Chou went on to report, “The term ‘skeletal muscle relaxants’ refers to a diverse collection of pharmacologically unrelated medications, grouped together because they are approved by regulatory agencies for treatment of spasticity or for musculoskeletal conditions such as tension, headache or back pain.” They are drugs that have been long studied and the effects and side effects have been well documented. Van Tudlar, Touray, Furlan, Solway, and Bouter (2003) concluded that, “Muscle relaxants are effective in the management of nonspecific low back pain, but the adverse effects require that they be used with caution”(p. 1978).
As mentioned, low back pain is one of the most common conditions encountered in clinical practice and medications are the most commonly used type of treatment, and muscle relaxers are a common drug that has been prescribed by medical doctors for years for nonspecific low back pain, according to Chou (2010). Chou went on to report, “The term ‘skeletal muscle relaxants’ refers to a diverse collection of pharmacologically unrelated medications, grouped together because they are approved by regulatory agencies for treatment of spasticity or for musculoskeletal conditions such as tension, headache or back pain.” They are drugs that have been long studied and the effects and side effects have been well documented. Van Tudlar, Touray, Furlan, Solway, and Bouter (2003) concluded that, “Muscle relaxants are effective in the management of nonspecific low back pain, but the adverse effects require that they be used with caution”(p. 1978).

 Molecular Neurobiology
Molecular Neurobiology B) An increase in saturated fat
B) An increase in saturated fat
 Journal of the American Board of Family Medicine
Journal of the American Board of Family Medicine
 Improvement of Chronic Back Pain or Failed Back Surgery with Vitamin D Repletion: A Case Series
Improvement of Chronic Back Pain or Failed Back Surgery with Vitamin D Repletion: A Case Series
 On the Aetiology of Autism
On the Aetiology of Autism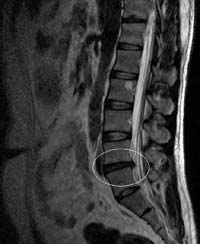
 Journal of Bone and Joint Surgery (American)
Journal of Bone and Joint Surgery (American)