Computerized Diagnostic Technology
by Aaron Ford, D.C.
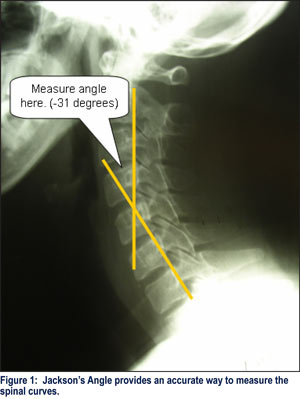
Radiographic distortion has been a cause of disagreement together with the compounding inaccuracy of manual line drawing. Not mentioned, however, is the fact that computer technology has become available that is capable of recalculating the configuration of the spine, thereby correcting vertebral anatomy to its proper size and scale, as well as marking precise lines and providing exact measurements.
A simple analogy is to explain that the newly manufactured automobiles have engineered crumple zones designed into the belly-pan that supports the body of the car. If this car were to be in a front or rear-end collision, the vehicle would be sent to a body shop. Depending upon the manufacturers, there are pre-engineered salient points that are marked on the belly-pan for the purpose of measurement. Laser beams are set between these points and measurements are taken. If these measurements exceed specific tolerances, then this vehicle is removed from the nation’s highways.
X-ray digitization software analyzes and measures the salient points on the human body’s framework, the spine. If the tolerances are exceeded, according to the AMA Guidelines to the Evaluation of Permanent Impairment, the patient is offered a 25 percent whole person impairment. This is where we can document a permanency of the injury that requires ongoing chiropractic care.
Dr. Chung Ha Suh, chairman of the department of mechanical engineering at the University of Colorado (Boulder), developed the first software during the 1970’s and, by 1984, presided over the 15th annual Biomechanics Conference, held in his homeland of Korea, devoted to computer graphics.
Dr. Suh originated the algorithms necessary to correct for 99 percent of the distortion on plain film X-rays. Moreover, the software programs incorporate most commonly used line drawings, so that these are also reproducible with a precision and exactness impossible to achieve manually, especially in the hectic surroundings of a working clinic.
Computerized Spinographic analysis is used by chiropractors to objectively analyze the biomechanical improprieties of the spine. (Rome) It is medically necessary to assess the degree to which an injury has affected the patient’s health and future well being; i.e., an impairment rating.
Imaging methods shall be utilized for obtaining information concerning the vertebral subluxation and other malpositioned articulating structures and ligamentous instability (sub-failure) during motion. Chiropractic concerns are primarily the spinal misalignment component, although advanced imaging can also provide valuable information regarding foraminal alteration, nerve impingement, and aberrant motion.
Spinal X-rays are deemed appropriate when the patient’s history and subjective complaints indicate a probable musculoskeletal involvement. Computerized Spinographic analysis is clearly called for in order to undertake biomechanical analyses involving small units of measurement (millimeters and degrees), in order to arrive at a differential diagnosis, or to determine treatment protocols, besides providing a definitive baseline for follow-up radiological examinations.
The insurance industry requires three things:
1. Was the patient injured on a more probable or not basis?
2. Is there objective evidence to validate the injury?
3. Can an objective based treatment plan be designed in an attempt to return the patient to pre-injury status?
These are logical and legitimate questions that a third-party payer requires. If the doctor can accomplish these three steps, they will be less likely to have the treatment prematurely terminated.
Dynamic Motion X-ray and digitizing provides the chiropractor with the best possible information on the biomechanical status of a patient’s spine. The informed chiropractor can accurately assess the patient and, as an added, educational (and motivational) bonus, the patient can visualize his/her structural improprieties when that spine is compared to the standard spine, side-by-side. This process, additionally, empowers patients in their own treatment plans, enabling them to view the desired anatomical goal, as well as boosting motivational levels to persevere through the often-tedious rehabilitation process; especially, if a time frame is established, and each progressive stage is met from the outset.
Digitizing follow-up X-rays again utilizes scientific imaging analysis to determine treatment progress, or lack thereof, assisting the chiropractor in assessing the efficacy of the treatment protocol and associated needs (including: therapy, rehabilitation, reducing job activity). It further assists in arriving at a more accurate impairment assessment or, as a last resort, determining actual levels of permanent impairments in those patients who will not completely recover from their injuries.
While it remains true that the technological explosion in health care delivery has advanced far beyond valid clinical utility, no matter how many instruments become available, the key device in chiropractic diagnosis remains the X-ray machine. Indeed, in virtually every state, a chiropractor is specifically required by the state legislature to be responsible for the diagnosis of vertebral subluxations (or other synonyms) from X-ray analysis.
More recently (Smith versus Yohe, Supreme Court of Pennsylvania, 1963) negligence was confirmed after a failure to take X-rays.
“If a physician, as an aid to his diagnosis (i.e., his judgment) does not avail himself of the scientific means and facilities open to him for the collection of the best factual data upon which to arrive at his diagnosis, the result is not an error of judgment but negligence in failing to secure an adequate factual basis upon which to support his diagnosis or judgment.”
If we may speculate on the near future, merely taking X-rays is not going to be the end of the story. While, of course, it is implied that anyone taking an X-ray would have diagnosed the conditions due to biomechanical improprieties, remembering that negligence applies to things that were left undone, one can consider a condition requiring a precise measurement of the X-ray, such as Alteration of Motion Segment Integrity. If utilization of computer digitization to analyze and measure spinal subluxation becomes an established clinical procedure, then it will become the gold standard for such measurements.
One might conclude, then, that: computerized digitization of plain film X-rays is not just a matter of clinical efficacy but a clinical necessity. (Cockburn)
Bould’s study found the human eye calibration of a digital caliper to be accurate to 0.26 mm and reproducible to +/-0.1mm. The resolution of the caliper is given as 0.01 mm and it is certified for 0.02+/- mm.
Bould, also, succinctly points out that accuracy requires the elimination of errors. If we are confronted by a known error, as with radiographic distortion, it must be corrected in order to achieve accuracy of the measurement.
The Dynamic X-ray Analyzer (DXAnalyzer©) software model has the ability to perform statistical evaluations of inter- and intra-examiner reliability studies and has been tested and found to be accurate to 0.0023mm, which assures that injured patients receive the best digital spinal analysis available. This system is designed to digitize any known format of X-ray image and correct for the 30 percent error in X-ray image distortion for Focal Film Distance and Object Film Distance to less than 1 percent error, simultaneously, from any known image source. The DX Analyzer has an interactive database to include: patient’s age, height, weight, gender, and genetic heritage. Chiropractic can now be made bullet proof when qualifying and quantifying spinal injuries and subluxations.
The term “qualifying” refers to the ability of the computer to identify the true landmarks, ignoring any subjective misperceptions, and erroneous markings. (Bellamy)
The term “quantifying,” of course, refers to the property of things that can be measured. Included measurements are:
Motion segment integrity—angular
Motion segment integrity—translation
The Guideline Protocol for Radiographic Digitization was established for undertaking radiographic digitization:
1. When examination findings are equivocal and radiographs have been taken, in the presence of apparent normal radiographic findings.
2. When a patient’s symptoms do not agree with examination findings and X-rays are deemed necessary and may rule out or detect factual presence of a biomechanical instability.
3. When a patient is not responding favorably to care and a degenerative or insidious process is suspected.
4. When biomechanical information is deemed helpful in the direction of the treatment plan.
5. When assistance may be necessary in assessing activities of daily living, temporary or permanent disability or in apportionment issues.
6. In determining progress or lack of it in a condition, this has required post-radiographic examination of the patient.
This digital analysis of a specific X-ray produces an outcome assessment process which helps establish the following:
1. A diagnosis for the correction of specific motion segments and functional units.
2. A scale to assess the patient’s current condition, compare serial studies and determine maximum clinical improvement.
3. A specific treatment plan, with the clinical goal of restoration of the patient’s functional biomechanics.
4. Unique graphical information of the patient’s biomechanical findings for at-a-glance reference in establishing the treatment plan.
5. A reference norm.
6. A line drawing or graphical measurement (depending upon the analysis selected).
7. A bar graph (depending upon the analysis selected).
A practice that utilizes computer-aided X-ray digitization analysis might lead to an increase in the number of patients with positive X-ray findings, as well as positive diagnoses. Indeed, as the experience with the protocol increases, one might conjecture that patients will begin to utilize the chiropractic profession more readily, based upon its ability to provide more accurate objective diagnoses.
It is imperative that today’s practicing chiropractor keep abreast of the advancement in imaging technology and measurement analysis. During the 1980’s, we were obligated to identify the patient’s name and policy number and summarily submit a bill. Today, the call is for fraud investigation based on inadequate documentation and the use of “special investigative units,” of which the number has tripled, to perform post-payment reviews. Utilizing evidence-based, objective documentation will demonstrate a responsible position of the attending chiropractor to establish what is reasonable and necessary for his/her care.
Aaron Ford, D.C., is a 1998 graduate of Parker College of Chiropractic. He is the Managing Director of Digital Spinal Diagnostics, the only digitizing service company to utilize the DXAnalyzer© X-ray digitizing software, which is compliant with the AMA Guidelines to the Evaluation of Permanent Impairment, 4th, 5th, and 6th Editions. To request more information on diagnostic computer-aided X-ray digitization services, call 1-866-608-4373 or link to www.digitalspinaldiagnostics.com.
 Static sEMG shares similar concerns with regards to reproducibility. Patient position, user training and proper test technique are as important with Static sEMG as with BP. And clinical value parallels BP measures in the world of spinal health. When viewed in context over a period of time, patterns of muscular compensation clearly emerge providing valuable clinically meaningful, spinal-specific data to aid the Chiropractor and patient in determining need for care and tracking of progress. It is however crucial that one utilize proper equipment, test protocol and consider individual patient variables (e.g. height, medication, exercise) when interpreting results. At minimum, think of Static sEMG as an electronic form of palpation. It augments palpation by providing purely objective data which unlike palpation is quantifiable.
Static sEMG shares similar concerns with regards to reproducibility. Patient position, user training and proper test technique are as important with Static sEMG as with BP. And clinical value parallels BP measures in the world of spinal health. When viewed in context over a period of time, patterns of muscular compensation clearly emerge providing valuable clinically meaningful, spinal-specific data to aid the Chiropractor and patient in determining need for care and tracking of progress. It is however crucial that one utilize proper equipment, test protocol and consider individual patient variables (e.g. height, medication, exercise) when interpreting results. At minimum, think of Static sEMG as an electronic form of palpation. It augments palpation by providing purely objective data which unlike palpation is quantifiable. 

 But today you no longer have to go the manual route, with relatively inexpensive automated systems where the entire process can be reduced – both testing AND reporting – to an average of mere minutes.
But today you no longer have to go the manual route, with relatively inexpensive automated systems where the entire process can be reduced – both testing AND reporting – to an average of mere minutes.
 NCS without EMG’s are considered experimental by most insurance companies, which is why you have seen a recent trend in companies now offering NCS and needle EMG; however, many are hiring and training physicians (including chiropractors) who take a weekend training course. Again, this raises questions as to the understanding and expertise of the person performing the test, and unless a competent exam is being performed you may again be exposing yourself to liability. In addition, many states require the use of the 6th Ed. of the AMA Guides to Impairment of Permanent Injury and this text clearly explains that in order to impair and rate a radiculopathy you must have “needle” EMG evidence (pgs. 579-580). Please do not get drawn in by the allure of Somato Sensory Evoked Potentials (SSEPs) or Dermatome Evoked Potentials (DEPs) as they are not medically necessary in the vast majority of cases.
NCS without EMG’s are considered experimental by most insurance companies, which is why you have seen a recent trend in companies now offering NCS and needle EMG; however, many are hiring and training physicians (including chiropractors) who take a weekend training course. Again, this raises questions as to the understanding and expertise of the person performing the test, and unless a competent exam is being performed you may again be exposing yourself to liability. In addition, many states require the use of the 6th Ed. of the AMA Guides to Impairment of Permanent Injury and this text clearly explains that in order to impair and rate a radiculopathy you must have “needle” EMG evidence (pgs. 579-580). Please do not get drawn in by the allure of Somato Sensory Evoked Potentials (SSEPs) or Dermatome Evoked Potentials (DEPs) as they are not medically necessary in the vast majority of cases.

 The primary cause is from overstressing a particular muscle group or joint. Your muscles and joints become accustomed to the repetitive movement patterns in which you place your neuro-musculoskeletal system. Does the term “muscle memory” ring a bell? When you do a new workout or activity that causes those muscles and joints to be used in a different pattern of movement, your muscle tissue must respond. We all have heard of the physical stress theory or the theory of adaptation and Wolf’s law. It is easy for our patients to understand why they have the soreness after bending over and picking up sticks from their yard after a wind storm if they normally do very little bending as part of their activities of daily living. Or if the patient typically has a sedimentary lifestyle and begins an exercise program, there is usually no questioning why he or she is sore. Keep in mind when you recommend an exercise program to patients that they may be hesitant on beginning it if they have experienced delayed onset muscles soreness before and remember it to be a painful experience.
The primary cause is from overstressing a particular muscle group or joint. Your muscles and joints become accustomed to the repetitive movement patterns in which you place your neuro-musculoskeletal system. Does the term “muscle memory” ring a bell? When you do a new workout or activity that causes those muscles and joints to be used in a different pattern of movement, your muscle tissue must respond. We all have heard of the physical stress theory or the theory of adaptation and Wolf’s law. It is easy for our patients to understand why they have the soreness after bending over and picking up sticks from their yard after a wind storm if they normally do very little bending as part of their activities of daily living. Or if the patient typically has a sedimentary lifestyle and begins an exercise program, there is usually no questioning why he or she is sore. Keep in mind when you recommend an exercise program to patients that they may be hesitant on beginning it if they have experienced delayed onset muscles soreness before and remember it to be a painful experience.





 If you are like many other doctors or students interested in nutrition, you must be able to determine when you should adjust physically or when a chemical adjustment is needed to keep that physical adjustment in place. Whether it is from
If you are like many other doctors or students interested in nutrition, you must be able to determine when you should adjust physically or when a chemical adjustment is needed to keep that physical adjustment in place. Whether it is from