History
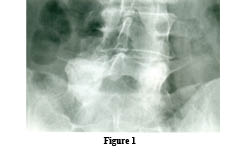
HistoryThis 60-year-old female patient presents with lower back and sciatica pain through the buttock into the posterior thigh.
Diagnosis:
Observe the extensive sclerosis and osteophyte formation occurring bilaterally at the L5/S1 facet structures. There is a degenerative anterolisthesis of L5 upon the sacrum of approximately 4 mm. No evidence of pars defects is seen at the L5 segment.
Degenerative Spondylolisthesis:
 Degenerative spondylolisthesis is a type of non-spondylolytic spondylolisthesis (no pars defect). Schmorl and Junghans refer to this condition as “pseudo-spondylolisthesis” to differentiate it from cases with a neural arch defect (spondylolytic spondylolisthesis). Macnab prefers the phrase “spondylolisthesis with an intact neural arch,” which is a more accurate description.¹
Degenerative spondylolisthesis is a type of non-spondylolytic spondylolisthesis (no pars defect). Schmorl and Junghans refer to this condition as “pseudo-spondylolisthesis” to differentiate it from cases with a neural arch defect (spondylolytic spondylolisthesis). Macnab prefers the phrase “spondylolisthesis with an intact neural arch,” which is a more accurate description.¹Degenerative spondylolisthesis can affect any degenerated vertebral segment positioned within a lordotic curve. In the lumbar spine, it most commonly affects L4, with approximately 10 times more prevalence than at the L3 or L5 vertebrae. Generally, anterior displacement of the L4 vertebral body is not > 25%, and the majority of cases involve only 10-15% displacement. ¹
Degenerative spondylolisthesis is a forward displacement of a vertebral body secondary to extensive superior and inferior facet arthrosis. This is frequently associated with degenerative disc disease and is most commonly found at the L4 segment in females > 40 years of age (the three Fs of degenerative spondylolisthesis).¹
The Three F’s Of Degenerative Spondylolisthesis
- Female
- Fourth lumbar vertebra
- Forty years old or older 1
The absence of a pars defect (which would increase the sagittal dimensions of the central canal) results in narrowing of the antero-posterior (AP) diameter of the spinal canal, which causes central spinal stenosis, in addition to lateral recess and neuroforaminal stenosis. The contours of the thecal sac have an hourglass or cosntrictred outline. Because the vertebral body projects anterior and inferior in relation to the disc below, a pseudo-disc appearance can be created on the CT or MRI studies.¹
Synovial Cyst Formation
Synovial cysts are degenerative in nature and can occur in or adjacent to degenerative facet joints. They may reach considerable size and cause localized back and leg pain. On T1-weighted images, synovial cysts may be seen as low signal intensity masses in the posterior spinal canal. They may be better delineated on T2-weighted scans because their fluid contents become hyperintense. The key to the diagnosis is their location and the proximity of the cyst to the synovial joint. Although an unusual finding, gas-filled synovial cysts have been reported. This degenerative vacuum phenomenon may be present in the apophyseal joint, and the continuity of cysts within the synovial joint can allow gas to become trapped within the cyst.¹
Clinical Comment And Summary:
Patients with degenerative spondylolisthesis who present with not only back pain but also ongoing leg pain that does not resolve with conservative treatment should be evaluated by an MRI scan to rule out a degenerative synovial cyst. These cysts can compress the exiting nerve root and produce unremitting leg pain. Cox has described reduction of these cysts with flexion distraction treatment as was documented by the work of Wilby on blockage of the 12 mm drainage opening from the facet joint to the ligamentum flavum as the cause of the cyst. ² Cox has reported a number of cases where there has been successful decompression of these cysts with flexion distraction treatment.3,4,5 Surgical intervention has also been recommended to remove the cysts rather than just decompress the cysts by means of puncture. Without surgical removal, the cysts often recur similar to a Baker’s cyst recurring in the knee.
References
- Yochum TR, Rowe LJ: The Essentials of Skeletal Radiology, 3rd ed., Baltimore, Williams & Wilkins, 2005.
- Martin J. Wilby, Robert D. Fraser, Barrie Vernon-Roberts and Robert J. Moore: SPINE, Volume 34, Number 23, pp. 2518-2524.
- James Cox, Chiropractic Treatment of Lumbar Spine Synovial Cysts: A Report of Two Cases, J. Manipulative and Physiological Therapeutics.28(2), Feb. 2005, p. 143-147.
- James Cox, Chiropractic Treatment of Lumbar Spine Synovial Cysts: A Report of Two Cases, J. Manipulative and Physiological Therapeutics.28(2), Feb. 2005, p. 143-147.
- L. Hazen, James Cox: Lumbar Intraspinal Extradural Synovial Cyst: A Case Study, J. Neuromusculoskeletal System, 1(4): 1993.
Dr. Terry R. Yochum is a second generation chiropractor and a Cum Laude Graduate of National College of Chiropractic, where he subsequently completed his radiology residency. He is currently Director of the Rocky Mountain Chiropractic Radiological Center in Denver, Colorado, and Adjunct Professor of Radiology at the Southern California University of Health Sciences, as well as an instructor of skeletal radiology at the University of Colorado School of Medicine, Denver, CO. Dr. Yochum can be reached at 1-303-940-9400 or by e-mail at [email protected]
Dr. Alicia M. Yochum is a third generation chiropractor and 2011 Suma Cum Laude Graduate of Logan College of Chiropractic, as well as a Registered Nurse. She is in a Radiology residency at Logan College in St. Louis, MO. She can be reached at [email protected].