 Herein lies multiple potential culprits for an inaccurate diagnosis. First, as I have discussed previously, general radiologists have a 42.2% error rate as reported by Lurie, Doman, Spratt, Tosteson, and Weinstein (2009), which makes it virtually imperitive that we, as practitioners, must take control of a critical component in diagnosing our pateints. At the very least, we must understand the basics of MRI spine interpretation to verify the findings or lack thereof. We also must be congnizant of the fact that we often rely on the MRI when ordering and delivering high velocity thrusts into our pateints. At this level, accuracy matters in determining a correct prognosis and treatment plan to ensure the safety of our patients when adjusting the spine. It is imperative for chiropractic.
Herein lies multiple potential culprits for an inaccurate diagnosis. First, as I have discussed previously, general radiologists have a 42.2% error rate as reported by Lurie, Doman, Spratt, Tosteson, and Weinstein (2009), which makes it virtually imperitive that we, as practitioners, must take control of a critical component in diagnosing our pateints. At the very least, we must understand the basics of MRI spine interpretation to verify the findings or lack thereof. We also must be congnizant of the fact that we often rely on the MRI when ordering and delivering high velocity thrusts into our pateints. At this level, accuracy matters in determining a correct prognosis and treatment plan to ensure the safety of our patients when adjusting the spine. It is imperative for chiropractic.Slice thickness is another critical component of a quality MRI. The American College of Radiology (ACR) has set forth the following guidelines for maximum thicknesses:
 The key to this graph is the concept “maximum” and it does not illustrate a complete sequence to ensure that most pathologies are not missed. In addition, most MRI centers tout that they are ACR accredited and that is factual. However, being ACR accredited does not mean that they use ACR guidelines in their scans. In addition, there are no regulatory standards in any state enforcing those guidelines for imaging centers. That “ruse” is quite profitable for those centers at both you and your patients’ expense because this often leads to many missed pathologies. So it also leaves you exposed to hurting your patients—caveat emptor!
The key to this graph is the concept “maximum” and it does not illustrate a complete sequence to ensure that most pathologies are not missed. In addition, most MRI centers tout that they are ACR accredited and that is factual. However, being ACR accredited does not mean that they use ACR guidelines in their scans. In addition, there are no regulatory standards in any state enforcing those guidelines for imaging centers. That “ruse” is quite profitable for those centers at both you and your patients’ expense because this often leads to many missed pathologies. So it also leaves you exposed to hurting your patients—caveat emptor!
According to Robert Peyster, MD, neuroradiologist and section chief of neuroradiology of State University of New York at Stony Brook Medicine who acquired his neuroradiology education at Mass General (Harvard) and has been published more than sixty times on MRI, the following sequences should be considered:
 Please note that all of the scenarios involve “no gap.” They are no longer necessary with today’s technology. These recommendations exceed the ACR guidelines and are meant to do so. As I have already articulated, those guidelines are minimum standards with maximum slice thicknesses. The thinner the slice, the more you see with “volume averaging” in image acquisition.
Please note that all of the scenarios involve “no gap.” They are no longer necessary with today’s technology. These recommendations exceed the ACR guidelines and are meant to do so. As I have already articulated, those guidelines are minimum standards with maximum slice thicknesses. The thinner the slice, the more you see with “volume averaging” in image acquisition.
Understanding that this article is intended to serve as a guide, I urge every DC worldwide to learn the significance of each sequence and be able to interpret MRIs (or at least the basics) to protect patients from any of the above scenarios. Dr. Peyster and other world-class specialists teach MRI to DCs at www.teachdoctors.com. This course carries a certification from the University of Bridgeport, College of Chiropractic and State University of New York at Buffalo, School of Medicine and Biomedical Sciences. This is the only program that offers a “cross certification” through both chiropractic and medical academia. Although this has had significant positive ramifications for chiropractic in the courts nationally by allowing DCs to testify as experts when challenged, the real winners are the patients.
Do not be taken advantage of by unscrupulous imaging centers when ordering MRIs. Winning through clinical excellence is the only solution and DCs now have the opportunity to learn how to interpret MRIs from the same educators who have taught thousands of medical neuroradiologists to interpret spinal MRIs. This level of clinical excellence has nothing to do with your philosophy of practice or method of delivery of care. It is purely about accurately triaging your patients with an accurate diagnosis, prognosis, and treatment plan.
References:
- Lurie, J. D., Doman, D. M., Spratt, K. F., Tosteson, A. N. A., & Weinstein, J. N. (2009). Magnetic resonance imaging interpretation in patients with symptomatic lumbar spine disc herniations. Spine, 34(7), 701-705.
- American College of Radiology (2011). MRI practice guideline for the performance of magnetic resonance imaging (MRI) of the adult spine. Last retrieved July 11, 2013 from http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/MRI_Adult_Spine.pdf

 History
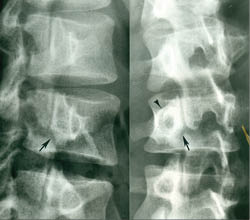
History Degenerative spondylolisthesis is a type of non-spondylolytic spondylolisthesis (no pars defect). Schmorl and Junghans refer to this condition as “pseudo-spondylolisthesis” to differentiate it from cases with a neural arch defect (spondylolytic spondylolisthesis). Macnab prefers the phrase “spondylolisthesis with an intact neural arch,” which is a more accurate description.¹
Degenerative spondylolisthesis is a type of non-spondylolytic spondylolisthesis (no pars defect). Schmorl and Junghans refer to this condition as “pseudo-spondylolisthesis” to differentiate it from cases with a neural arch defect (spondylolytic spondylolisthesis). Macnab prefers the phrase “spondylolisthesis with an intact neural arch,” which is a more accurate description.¹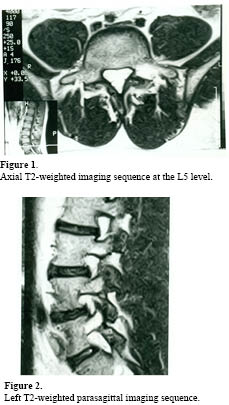
 Historically, two modes of diagnostic imaging have been used to assess whether physiological activity is present and associated with the existing pars defects or “PENDING” defects. Radionuclide bone scan imaging, particularly SPECT (Single Photon Emission Computed Tomography), has often been the examination of choice; however, it suffers from two drawbacks: it exposes the patient to ionizing radiation and it provides very little anatomical information. Fortunately, these concerns have been addressed with the advent of MR imaging. Understanding that pars defects represent a stress fracture of the fatigue variety rather than an inherited congenital anomaly or predisposition has been a life-long quest for me (Terry R. Yochum). Having reviewed many athletes’ images, I have had the opportunity to see the proven value of MR imaging for the assessment of physiological activity that occurs adjacent to a pars defect, or that which is hidden in the region of the pars interarticularis when the defect is in fact “PENDING.” I feel, at this point in time, that SPECT imaging is no longer the exam of choice, since there is so much more information obtained with the physiological imaging of magnetic resonance.
Historically, two modes of diagnostic imaging have been used to assess whether physiological activity is present and associated with the existing pars defects or “PENDING” defects. Radionuclide bone scan imaging, particularly SPECT (Single Photon Emission Computed Tomography), has often been the examination of choice; however, it suffers from two drawbacks: it exposes the patient to ionizing radiation and it provides very little anatomical information. Fortunately, these concerns have been addressed with the advent of MR imaging. Understanding that pars defects represent a stress fracture of the fatigue variety rather than an inherited congenital anomaly or predisposition has been a life-long quest for me (Terry R. Yochum). Having reviewed many athletes’ images, I have had the opportunity to see the proven value of MR imaging for the assessment of physiological activity that occurs adjacent to a pars defect, or that which is hidden in the region of the pars interarticularis when the defect is in fact “PENDING.” I feel, at this point in time, that SPECT imaging is no longer the exam of choice, since there is so much more information obtained with the physiological imaging of magnetic resonance.
 Case History: This male patient was working on the roof of his garage when he slipped and fell 12 feet to the concrete pavement of his driveway. He has sharp pain over his proximal sacrum. Does he have a fracture?
Case History: This male patient was working on the roof of his garage when he slipped and fell 12 feet to the concrete pavement of his driveway. He has sharp pain over his proximal sacrum. Does he have a fracture?


 Computed radiography (CR) is the closest process to traditional radiography because it still includes the use of X-ray cassettes and films, albeit in a different form. Instead of the traditional X-ray film, computed radiography makes use of a reusable phosphor plate. After taking each image, the plate will be processed through a scanner that then erases the image so that the plate can be used again. As the process of obtaining imaging is very similar to traditional radiography, computed radiography also takes the same time to finish one cycle.
Computed radiography (CR) is the closest process to traditional radiography because it still includes the use of X-ray cassettes and films, albeit in a different form. Instead of the traditional X-ray film, computed radiography makes use of a reusable phosphor plate. After taking each image, the plate will be processed through a scanner that then erases the image so that the plate can be used again. As the process of obtaining imaging is very similar to traditional radiography, computed radiography also takes the same time to finish one cycle. 
 [Case History]
[Case History]

 [Case History]
[Case History]
 Appear modern, cutting edge, and up-to-speed with other health care practices. Patients are turned off when walking into a practice that appears to be circa 1975. They simply don’t feel comfortable with a “tired” atmosphere, complete with old adjustment tables with torn padding.
Appear modern, cutting edge, and up-to-speed with other health care practices. Patients are turned off when walking into a practice that appears to be circa 1975. They simply don’t feel comfortable with a “tired” atmosphere, complete with old adjustment tables with torn padding.  Patient education, compliance and retention
Patient education, compliance and retention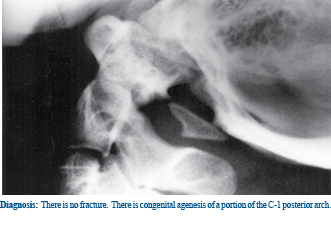
 [Case History]
[Case History]