 :dropcap_open:W:dropcap_close:e all are victims, in many ways, of the existing healthcare crisis. The auto industry is addressing their crisis through new laws for improved mileage per gallon and stricter pollution controls. The energy crisis continues to search for more efficient and alternative means to produce renewable energy. The healthcare crisis, unlike the above two, is merely shifting responsibilities with regard to who will pay for it. This “system” will continue until it can no longer sustain itself.
:dropcap_open:W:dropcap_close:e all are victims, in many ways, of the existing healthcare crisis. The auto industry is addressing their crisis through new laws for improved mileage per gallon and stricter pollution controls. The energy crisis continues to search for more efficient and alternative means to produce renewable energy. The healthcare crisis, unlike the above two, is merely shifting responsibilities with regard to who will pay for it. This “system” will continue until it can no longer sustain itself.
Chiropractic’s Role
As chiropractors, we are interested in the neuro-musculo-skeletal system (NMS). The current healthcare system has 3 major flaws in addressing NMS disorders: 1) We wait until someone breaks, 2) we only look at the sight of the break, and 3) our goal is only to remove the pain or symptoms. This approach costs exponentially more, as we all know it is less expensive to “pay now” vs. “pay later,” especially when the proactive approach will produce slower aging, delayed degeneration and a much greater quality of life. Joint replacement surgery is a growth industry. It doubled between 2000 and 2006. Osteoarthritis, the leading arthritis, better known as the wear and tear arthritis, is predicted to have costs and numbers rise by 40% by 2030.
As chiropractors, we know that a joint that has lost mobility is predisposed to a more rapid degeneration. We know that joints will fixate when under greater stress (abnormal mechanical loading), such as with traumas or biomechanical imbalances. These fixations prevent people from moving or exercising, which is the breeding ground for obesity, elevated blood pressure, increased anxieties, elevated cholesterol and much more. We know that we, as a profession, are the most equipped to both detect and improve biomechanical fixations and imbalances. This approach will make a dramatic impact on the “fixing” of this healthcare crisis.
Altered Biomechanics and Bone Marrow Edema?
According to an article published in the journal Radiology 1996 by Mark E. Schweitzer, M.D., and Lawrence M. White, M.D., from Thomas Jefferson University Hospital in Philadelphia, PA, a very unique study was performed to evaluate the effects of altered biomechanical stress on the human skeleton. The details of this study are as follows:
» Twelve asymptomatic volunteers (6 women and 6 men) ranging between the ages of 19 and 41 were chosen to be evaluated in this biomechanical study. All 12 of these asymptomatic volunteers had MR images of their hips, knees, ankles and feet performed at the initial time of commencement of the study. No evidence of pathology or bone marrow edema was seen affecting any of these 12 volunteers and the MR imaging was done bilaterally. Three sets of images were obtained before, baseline and 2 weeks after altered weight bearing and then 3 volunteers two weeks after removal of a pad, which had forced the patient into altered biomechanical weight bearing. The alteration in weight bearing was accomplished by placing an extra large 9/16” (1.4 cm) longitudinal metatarsal arch pad underneath the lateral aspect of one foot to increase pronation. This orthotic was placed in the shoe, but the volunteers did not undergo casting with the foot in this position. Therefore, movement was altered somewhat voluntarily. The volunteers were instructed not to alter their daily or recreational activities in any way other than that caused by the pronation. The volunteers were given an adequate number of pads for all pairs of their shoes. The pads were placed unilaterally to minimize discomfort.1
:dropcap_open:We know that joints will fixate when under greater stress (abnormal mechanical loading), such as with traumas or biomechanical imbalances.:quoteleft_close:
» After 2 weeks of altered weight bearing, MR images of both the lower extremities were obtained in the STIR (short tau inversion recovery) or fluid sensitive or fat suppression images) imaging sequence. All three sets were done with STIR sequences.1
» The results of these MR images was that 11 of the 12 volunteers demonstrated bone marrow edema on the over pronated side in 10 of the volunteers. One of the volunteers with medial involvement had the findings only on the non over pronated side. These changes were seen most frequently in the foot, four metatarsals and calcaneus. Changes were predominately lateral in 6 volunteers. The tibia was affected in 3 volunteers, two proximally and one distally and in an additional 3 volunteers, the femur was involved, one affecting the proximal femur and two affecting the distal femur. Eleven of these 12 volunteers had pain directly over the areas where bone marrow edema was identified. At MR follow-up, after the pad was removed in two of the three volunteers, the MR images returned completely to normal but, in the third volunteer, MR images demonstrated minimal persistent edema with approximately 50% having been resolved. All of the volunteers were completely asymptomatic immediately after the pad removal and at clinical follow-up. (1 week, 1 month, 1 year)1
Bone is dynamic, undergoing hypertrophy in response to stress. Alternatively, after immobilization from casting or paralysis or in a gravity free environment, bone atrophy occurs. What was most interesting about this study is that bone marrow edema and symptoms directly over the area of edema were created with only 2 weeks of altered biomechanical weight bearing with over pronation of one foot. One wonders if there would be altered biomechanics (subluxation) of the lower extremity and/or the lumbar spine for an extended period of time, what kind of stress this would place on the human skeleton and what long-standing effects it could have on premature degenerative changes within the freely moveable joints of the spine and/or pelvis and lower extremities. The results of this study clearly shows that increased signal intensity on fluid sensitive images or STIR images (fat suppression images) can occur and may represent a bone contusion or bone bruise. The results of this study indicates that the increased signal intensity is the result of a bony response to the stress created upon it without actual fracture occurring. On the basis of Schweitzer’s study, I believe that the altered biomechanics should be added to the list of causes of increased intramedullary signal intensity on T2 and/or STIR weighted images.1,2
It is of interest to note that I (Dr. Yochum) personally interviewed Dr. Mark Schweitzer and asked him if any of these 12 volunteers had lower back pain and/or sacroiliac pain. He told me that those questions were never asked of these volunteers. From my chiropractic perspective, I would have to believe that a large number of these patients would have had sacroiliac and/or lower lumbar pain. It would have been interesting to perform pre and post MRI images of the bones adjacent to the sacroiliac joint and/or the lumbar facets to determine whether bone marrow edema could have been identified there as a result of the altered biomechanical stress from the disturbance of the lower kinetic chain.1,2
Imaging Bone Marrow Edema
Imaging stress to the human skeleton may be done by means of plain films, bone scan, CT or MRI scan. The most sensitive imaging modality to detect stress to the human skeleton reflected as bone marrow edema is magnetic resonance imaging. While bone scans can certainly reflect an increase in turnover of bone, they are not as sensitive as the 1% sensitivity of marrow change occurring with MRI scans. Understanding this concept becomes extremely important to evaluate the highly motivated athlete who may or may not have the presence of a spondylolysis and/or spondylolisthesis on plain film radiographs and may only be seen by means of magnetic resonance imaging scans. It is possible that a patient may have normal plain film radiographs, but yet have pain on extension and have, in fact, the early fatigue fracture (stress fracture) of spondylolysis and be hidden or “PENDING.” Since the plain film radiographs may not be sensitive enough to detect the “PENDING” spondylolysis or certainly not see edema adjacent to existing pars defects (spondylolysis), specialized physiologic imaging such as magnetic resonance imaging should be given clinical consideration.2
Since on standard MR imaging with standard T1- and T2-weighted images, it is quite possible that bone marrow edema may be missed on the T2-weighted image in a patient who may be “PENDING” without defect or in a patient with an existing pars defect, who may have bone marrow edema adjacent to the pars defect. With that being the case, it is important that an additional imaging series referred to a short tau inversion recovery (STIR) images, otherwise known as fluid sensitive images or fat suppression images, should be performed routinely in patients where there is a high suspicion of the possibility of a hidden or pending pars defect or bone marrow edema adjacent to an existing pars defect. The imaging sequence of choice, which should be added to the standard routine MRI scan, is a sagittal STIR imaging sequence, which will unequivocally rule in or out the possibility of bone marrow edema in the region of the pars interarticulares, with or without a defect.2
For further discussion in patient management and evaluation of the problematic cases of spondylolysis and/or spondylolisthesis in the lower lumbar spine and how it relates to the highly motivated athlete, please see chapter 5 of Dr. Yochum’s textbook, “Essentials of Skeletal Radiology” which is the 3rd edition published in 2005.2
Evidence Based
 The industry is pushing for all care to be evidence based. The irony is that under this heading, less imaging is encouraged. Less treatment is encouraged. And, in the end, less correction will have been done. The chiropractic profession would do well to redefine our identity, and associate itself closely with the detection and correction of biomechanical faults, an identity our forefathers fought hard to protect. We would then be the only profession whose goal would be to correct these structural imbalances (even in the absence of symptoms), and not just provide symptomatic care. This identity would enhance the public’s perception of our profession, as the public is begging for someone to help them achieve structural preservation, especially when this approach would improve their long-term quality of life.
The industry is pushing for all care to be evidence based. The irony is that under this heading, less imaging is encouraged. Less treatment is encouraged. And, in the end, less correction will have been done. The chiropractic profession would do well to redefine our identity, and associate itself closely with the detection and correction of biomechanical faults, an identity our forefathers fought hard to protect. We would then be the only profession whose goal would be to correct these structural imbalances (even in the absence of symptoms), and not just provide symptomatic care. This identity would enhance the public’s perception of our profession, as the public is begging for someone to help them achieve structural preservation, especially when this approach would improve their long-term quality of life.
In order to achieve this result, we must look at all people from a biomechanical perspective, as everyone has biomechanical faults and imbalances. Just as the orthodontist improves the alignment of the teeth long before problems occur, it’s easy to understand the benefit of doing this to the NMS system as well. As seen in Fig. 1, all people have biomechanical imbalances, and these imbalances always originate in the feet.
If we ignore the imbalances in the feet, we would be ignoring the importance of a balanced foundation. Introductory Architecture teaches the importance of a balanced foundation. This is the very reason our office puts every patient into custom orthotics at the beginning of all correction programs.
Biomechanics of Feet
 There are 3 arches in each foot, with each being critically important for providing foundational balance. Upon scanning of the feet (Fig. 2), it is easily detectable if any or all of these arches have fallen. Most patients have multiple fallen arches, when scanned in the standing position. In addition, aging, gravity and stress over time will encourage further falling of these arches, which will alter centers of gravity in each and every joint of the body. Abnormal centers of gravity, combined with aging, will further accelerate the degenerative process in joints.
There are 3 arches in each foot, with each being critically important for providing foundational balance. Upon scanning of the feet (Fig. 2), it is easily detectable if any or all of these arches have fallen. Most patients have multiple fallen arches, when scanned in the standing position. In addition, aging, gravity and stress over time will encourage further falling of these arches, which will alter centers of gravity in each and every joint of the body. Abnormal centers of gravity, combined with aging, will further accelerate the degenerative process in joints.
Custom Orthotics
The simple solution to current foot/structural imbalances as well as future structural weaknesses is to put the patient into flexible custom orthotics at the start of their corrective program. Regardless of whether the patient appears to have pronated, supinated or even normal arches, the digital foot scan will demonstrate that most people will have some degree of fallen arches, as well as imbalances with body weight distribution. Secondly, although we don’t test for this in our office, a significant percentage of people will over-pronate during the gait cycle, and this over-pronation is blocked with flexible custom orthotics. Many injuries, especially sports injuries, occur or are aggravated during this over-pronation phase.
After we digitally scan each patient, along with our explanation of Fig. 1 (Crooked Man), along with the explanation of the potential for acceleration of degeneration if left imbalanced, most people will excitedly agree to the inclusion of custom orthotics as soon as possible. All people have a similar lifetime goal: to have a higher quality of life combined with greater activity.
More patients wearing custom orthotics in your office will convert to improved clinical results, improved patient satisfaction and greater patient compliance. And, if an office can “manage” patients properly, patients will require new orthotics every two years, keeping more people engaged in active care. This truly is the beginning of making your practice more successful and fixing the healthcare crisis.
Dr. Terry R. Yochum is a second generation chiropractor and a Cum Laude Graduate of National College of Chiropractic, where he subsequently completed his radiology residency. He is currently Director of the Rocky Mountain Chiropractic Radiological Center in Denver, CO, and Adjunct Professor of Radiology at the Southern California University of Health Sciences, as well as an instructor of skeletal radiology at the University of Colorado School of Medicine, Denver, CO. Dr. Yochum can be reached at 1-303-940-9400 or by e-mail at [email protected].
Dr. Maggs currently practices full time, while also lecturing for Foot Levelers. He is the developer of The Structural Management® Program, as well as the 10 Week Webinar Series, “How to Build Your High School Athlete Practice.” He can be reached at 1-518-393-6566 or [email protected]. His website is www.StructuralManagement.com.
References:
1. Schweitzer, Mark E; White, Lawrence M., Radiology; 198:851-853, 1996.
2. Yochum, TR, Rowe LJ: Essentials of Skeletal Radiology, ed. 3, 2005, Chapter 5.
 CASE HISTORY
CASE HISTORY

 :dropcap_open:W:dropcap_close:e all are victims, in many ways, of the existing healthcare crisis. The auto industry is addressing their crisis through new laws for improved mileage per gallon and stricter pollution controls. The energy crisis continues to search for more efficient and alternative means to produce renewable energy. The healthcare crisis, unlike the above two, is merely shifting responsibilities with regard to who will pay for it. This “system” will continue until it can no longer sustain itself.
:dropcap_open:W:dropcap_close:e all are victims, in many ways, of the existing healthcare crisis. The auto industry is addressing their crisis through new laws for improved mileage per gallon and stricter pollution controls. The energy crisis continues to search for more efficient and alternative means to produce renewable energy. The healthcare crisis, unlike the above two, is merely shifting responsibilities with regard to who will pay for it. This “system” will continue until it can no longer sustain itself. The industry is pushing for all care to be evidence based. The irony is that under this heading, less imaging is encouraged. Less treatment is encouraged. And, in the end, less correction will have been done. The chiropractic profession would do well to redefine our identity, and associate itself closely with the detection and correction of biomechanical faults, an identity our forefathers fought hard to protect. We would then be the only profession whose goal would be to correct these structural imbalances (even in the absence of symptoms), and not just provide symptomatic care. This identity would enhance the public’s perception of our profession, as the public is begging for someone to help them achieve structural preservation, especially when this approach would improve their long-term quality of life.
The industry is pushing for all care to be evidence based. The irony is that under this heading, less imaging is encouraged. Less treatment is encouraged. And, in the end, less correction will have been done. The chiropractic profession would do well to redefine our identity, and associate itself closely with the detection and correction of biomechanical faults, an identity our forefathers fought hard to protect. We would then be the only profession whose goal would be to correct these structural imbalances (even in the absence of symptoms), and not just provide symptomatic care. This identity would enhance the public’s perception of our profession, as the public is begging for someone to help them achieve structural preservation, especially when this approach would improve their long-term quality of life. There are 3 arches in each foot, with each being critically important for providing foundational balance. Upon scanning of the feet (Fig. 2), it is easily detectable if any or all of these arches have fallen. Most patients have multiple fallen arches, when scanned in the standing position. In addition, aging, gravity and stress over time will encourage further falling of these arches, which will alter centers of gravity in each and every joint of the body. Abnormal centers of gravity, combined with aging, will further accelerate the degenerative process in joints.
There are 3 arches in each foot, with each being critically important for providing foundational balance. Upon scanning of the feet (Fig. 2), it is easily detectable if any or all of these arches have fallen. Most patients have multiple fallen arches, when scanned in the standing position. In addition, aging, gravity and stress over time will encourage further falling of these arches, which will alter centers of gravity in each and every joint of the body. Abnormal centers of gravity, combined with aging, will further accelerate the degenerative process in joints.



 What are the dollars and cents of going with digital X-ray opposed to conventional film? There is a front-loaded cost to digital radiography but, as an investment, digital radiography not only offers cost savings (no film, no chemicals, no processors), it can actually become a profit center. Going digital, X-ray moves from a cost per film, to a fixed cost—meaning that, dependent upon the number of X-rays that you take, it will make the practice a profit. As the doctor sees more patients, the cost of taking X-rays, per patient, actually decreases.
What are the dollars and cents of going with digital X-ray opposed to conventional film? There is a front-loaded cost to digital radiography but, as an investment, digital radiography not only offers cost savings (no film, no chemicals, no processors), it can actually become a profit center. Going digital, X-ray moves from a cost per film, to a fixed cost—meaning that, dependent upon the number of X-rays that you take, it will make the practice a profit. As the doctor sees more patients, the cost of taking X-rays, per patient, actually decreases.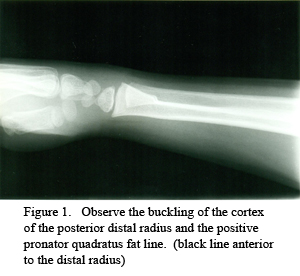

 :dropcap_open:I:dropcap_close:t is critical for every chiropractor to have a support team of health care specialists in order to render the highest level of care for our patients. The radiologist is the first specialist that you should add to your team. In the triaging of our patients, the progression is to create an accurate diagnosis, prognosis and treatment plan and then to treat. Imaging, both basic X-rays and advanced imaging such as MRI’s, CAT scans and bone scans are often a critical step in getting to “first base,” with the diagnosis. Without any diagnosis, we cannot treat our patients and, without an accurate diagnosis, we can go from spinal experts rendering quality care to well meaning practitioners who hurt their patients.
:dropcap_open:I:dropcap_close:t is critical for every chiropractor to have a support team of health care specialists in order to render the highest level of care for our patients. The radiologist is the first specialist that you should add to your team. In the triaging of our patients, the progression is to create an accurate diagnosis, prognosis and treatment plan and then to treat. Imaging, both basic X-rays and advanced imaging such as MRI’s, CAT scans and bone scans are often a critical step in getting to “first base,” with the diagnosis. Without any diagnosis, we cannot treat our patients and, without an accurate diagnosis, we can go from spinal experts rendering quality care to well meaning practitioners who hurt their patients.


