Case History
This 18-year-old female gymnast is complaining of unilateral left-sided lumbar spine pain at the L5 level. Standard plain film radiographs show no evidence of pathology, pars defects or spondylolisthesis. Because this patient’s pain did not respond to conservative treatment, an MRI scan was performed for further evaluation.
Imaging Findings of this Patient
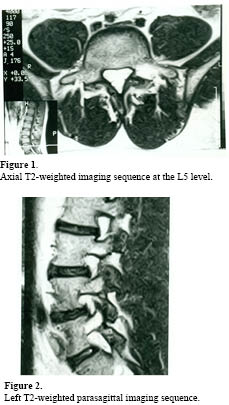
Observe the area of bright (white) signal intensity seen in the pedicle pars region on the left side at the L5 segment (arrows). This is nicely demonstrated on both the axial study and the left-sided parasagittal imaging. No true pars defects are identified at this time. The areas of increased signal intensity in the left pedicle pars region of L5 represent bone marrow edema and a “PENDING SPONDYLOLYSIS.” No pars defects were identified on the axial or parasagittal images. The author (Terry R. Yochum) has coined the term “PENDING SPONDYLOLYSIS” for those patients who are developing a stress fracture prior to any actual frank separation in the bone. If these patients continue to perform their repetitive hyperextension activities, the area where the bone marrow edema is present will cause the pars to actually fracture and separate.
Discussion
 Historically, two modes of diagnostic imaging have been used to assess whether physiological activity is present and associated with the existing pars defects or “PENDING” defects. Radionuclide bone scan imaging, particularly SPECT (Single Photon Emission Computed Tomography), has often been the examination of choice; however, it suffers from two drawbacks: it exposes the patient to ionizing radiation and it provides very little anatomical information. Fortunately, these concerns have been addressed with the advent of MR imaging. Understanding that pars defects represent a stress fracture of the fatigue variety rather than an inherited congenital anomaly or predisposition has been a life-long quest for me (Terry R. Yochum). Having reviewed many athletes’ images, I have had the opportunity to see the proven value of MR imaging for the assessment of physiological activity that occurs adjacent to a pars defect, or that which is hidden in the region of the pars interarticularis when the defect is in fact “PENDING.” I feel, at this point in time, that SPECT imaging is no longer the exam of choice, since there is so much more information obtained with the physiological imaging of magnetic resonance.
Historically, two modes of diagnostic imaging have been used to assess whether physiological activity is present and associated with the existing pars defects or “PENDING” defects. Radionuclide bone scan imaging, particularly SPECT (Single Photon Emission Computed Tomography), has often been the examination of choice; however, it suffers from two drawbacks: it exposes the patient to ionizing radiation and it provides very little anatomical information. Fortunately, these concerns have been addressed with the advent of MR imaging. Understanding that pars defects represent a stress fracture of the fatigue variety rather than an inherited congenital anomaly or predisposition has been a life-long quest for me (Terry R. Yochum). Having reviewed many athletes’ images, I have had the opportunity to see the proven value of MR imaging for the assessment of physiological activity that occurs adjacent to a pars defect, or that which is hidden in the region of the pars interarticularis when the defect is in fact “PENDING.” I feel, at this point in time, that SPECT imaging is no longer the exam of choice, since there is so much more information obtained with the physiological imaging of magnetic resonance.I have seen many cases where bone marrow edema adjacent to the pars or hidden within an intact pars on its way to becoming a pars defect (PENDING SPONDYLOLYSIS) has been missed on standard T2-weighted images. A STIR imaging sequence clearly provides this information. The STIR imaging sequences are the equivalent of fat suppression techniques or fluid-sensitive pulse sequences and significantly enhance the ability to see bone marrow edema within the region of the pars. If a STIR imaging sequence reveals bone marrow edema adjacent to an existing pars defect or within the pars interarticularis in a “PENDING SPONDYLOLYSIS,” patients must cease participating in any sports-related activities and be placed in a Boston Overlap brace for a minimum of three to four months. Once appropriately braced and physical activity is reduced, patients with “PENDING SPONDYLOLYSIS” usually do not develop a true bony pars defect.
The patient presented in this case study never developed actual pars defects and back pain was 90% reduced after being placed in a Boston Overlap brace for approximately three months. The patient’s lower back pain was 90% better once placed at a position of anti-lordosis, which is the purpose of the Boston Overlap brace.
For a more detailed discussion of this condition, its imaging evaluation, treatment and prognosis, please see Chapter 5 of the new edition of Yochum and Rowe’s Essentials of Skeletal Radiology published by Lippincott, Williams & Wilkins, 2005.
References
- Yochum TR, Rowe LJ: Essentials of Skeletal Radiology. 3rd ed. Baltimore MD): Lippincott, Williams & Wilkins; 2005.
Dr. Terry R. Yochum is a second generation chiropractor and a Cum Laude Graduate of National College of Chiropractic, where he subsequently completed his radiology residency. He is currently Director of the Rocky Mountain Chiropractic Radiological Center in Denver, Colorado, and Adjunct Professor of Radiology at the Southern California University of Health Sciences, as well as an instructor of skeletal radiology at the University of Colorado School of Medicine, Denver, CO. Dr. Yochum can be reached at 1-303-940-9400 or by e-mail at [email protected]
Dr. Alicia M. Yochum is a third generation chiropractor and 2011 Suma Cum Laude Graduate of Logan College of Chiropractic, as well as a Registered Nurse. She is in a Radiology residency at Logan College in St. Louis, MO. She can be reached at alicia.yochum@ gmail.com.