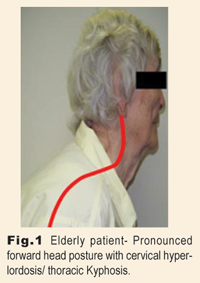
I recently got some great questions from a doctor in south Florida who frequently encounters aging patients with large forward head translations, yet have pronounced, sometimes even hyperlordotic, cervical curves. We’ve all observed this posture, common among elderly patients, but many doctors aren’t aware it needs to be managed differently than the typical case of FHP associated with cervical hypolordosis.

Typically, we find cervical HYPOlordosis and FHP occurring together. Normally, forward head translation occurs as the cervical lordosis is lost. Such cases typically present with disc degeneration beginning in middle age and progressing rapidly throughout the years. Advanced disc disease is quite common by age sixty in most such cases.
But, the cases I want to focus on today are actually quite different. These are individuals, typically older, in which the head appears to have translated forward without any accompanying loss of the cervical lordosis. In many of these cases, you will actually observe a HYPERlordotic cervical spine! This preservation of the lordosis seems to provide a great deal of protection from cervical disc degeneration even when degeneration is rampant throughout the rest of the spine. So what happens to make the progression so dramatically different? And what can we learn in order to better manage these unique postures?

The chicken or the egg?
From a structural perspective, the primary postural problem frequently seems to be a progressive thoracic kyphosis. It’s pretty easy to visualize how a relatively mild thoracic hyperkyphosis in youth, can gradually worsen with time. If kyphosis occurs prior to skeletal maturity, there is a tendency for wedging of the vertebrae to occur which may result in some degree of permanent deformation.1 As the hyperkyphosis progresses, the foundation for the cervical spine is tilted more forward and consequently, the patient’s head is literally forced to translate to the anterior. As the head translates forward, more anterior weight bearing stress is loaded onto the upper thoracic spine creating a cycle in which the kyphosis progresses over time. Compound these weight bearing factors with the common onset of osteoporosis in the elderly, and it starts to become clearer why many such patients will experience spontaneous anterior compression fractures in the thoracic spine. Many clinicians mistakenly assume that osteoporosis and resulting compression fracture are causal in this progression, but two thirds of patients with hyperkyphosis have no evidence of fracture…therefore the posture precedes the fractures not vice versa.2
Even as the posture gradually degrades, patients still have the need to keep their eyes level with their visual environment. The increased effort required to keep the head upright atop its precarious perch, results in continuous overloading of the posterior musculature. And while this commonly results in taut and painful traps and levator scapulae, it also works the cervical extensors so as to help accentuate the cervical lordosis. It is this preservation of the lordosis that serves to protect the mid cervical area from the degree of degeneration we might otherwise expect to see in aging patients.
Three useful tools for managing these postures.
In addition to the positive effects of your adjustments to reduce symptoms and improve mobility, 3 here are three more methods you may find useful to help reduce the amount of thoracic kyphosis, reduce forward head translation, and to reduce the mechanical workload of the posterior musculature.
1. Spinal Remodeling to reduce thoracic kyphosis. Daily session, 15-20 minutes minimum, over a roll or arch placed at the apex of the kyphosis. Start with 2-3 minutes and increase time as tolerated by patient. Depending on the severity of the kyphosis, it may be necessary to provide some head support for comfort.

2. Gentle long axis traction (over door/water bag type units are ideal for this) to lightly stretch SCM’s, reduce anterior weight bearing onto thoracic spine, and reduce slightly any cervical HYPERlordosis if present . (Note: Extension traction methods are NOT indicated on this type case. )

3. Reverse Posture Exercise: Patient performs posterior head translation exercise with roll or block behind thoracic spine. 8-10 repetitions per set, holding each contracture for 8-10 seconds. Strive for 3-4 sets daily as tolerated by patient.

Clinical Outcomes
Managing mild thoracic hyperkyphosis and FHP in young and middle aged patients is difficult enough. But, once those postures have become chronically entrenched in elderly, often deconditioned, patients, successful structural correction is much more problematic. Be realistic. Instead of striving for structural perfection, I suggest you reconsider what would constitute a satisfactory outcome. I’m quite happy in such cases to make some modest improvements in the patient’s thoracic kyphosis, reduce FHP to some degree, and relieve some of the chronic neck/shoulder pain and tension so common in these patients.
It’s important to be realistic when dealing with elderly patients. The ability of senior patients to achieve full correction is likely to be inhibited both by the chronicity of their condition as well as their own physical limits of participation in a structural rehab program. I strongly caution doctors to stay well within the limits of what is reasonably comfortable for your patients. Trying to push any patient too far beyond their comfort zone generally isn’t a good idea, but with elderly patients, it’s totally pointless. Just do what you can to help them, be realistic, and teach them what they can do to help themselves. In the end, most patients will appreciate your honesty and the practical nature of your approach.
Dr. Mark Payne is president of Matlin Mfg., a manufacturer and distributor of postural rehab products since 1988. A more detailed report on this subject is available for free, as well as a FREE SUBSCRIPTION to Postural Rehab...electronic newsletter on corrective chiropractic methods. CALL 334-448-1210 or email [email protected].
References
1. Nonsurgical treatment of kyphosis. Pizzutillo PD. Instr. Course Lect. 2004; 53 485-91 St. Christophers Hospital for Children. Philadelphia PA. PMID 15116637.
2. The rehabilitation of hyperkyphotic posture in the elderly. Kado DM. Eur J Phys Rehabil Med. 2009 Dec;45(4):583-93.
3. Rehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosis. Bautmans I, Van Arken J, Van Mackelenberg M, Mets T. J Rehabil Med. 2010 Feb;42(2):129-35.