What Scoliois Can Teach Us about Postural Rehab
:dropcap_open:M:dropcap_close:anifestation of any health problem is not a spontaneous event; before the clinical onset, precluding factors exist. Although these factors are unique in each patient, understanding how they contributed to the malady is the first step in reversing it. Regardless of the specific disorder, the crux of the issue is mal-adaptation: the body is adapting to demands placed upon it. When the ability of the body to adapt is exceeded, the result is overt symptomatology, often classified into a medically-recognized disorder.

Posture is a classic example of a condition which lacks a medical label to apply to it, but nonetheless has a dramatic effect upon health. Due to the fact that “poor posture” is not recognized as a medical condition, very little standardized research can be performed upon it, and this makes it difficult to understand its etiopathogenesis and the ideal methods to combat it. However, there are few diseases which have as strong an association with posture as scoliosis, and ongoing research on scoliosis may shed some light on the best strategies for patients suffering from imbalanced posture.
There can be numerous causes of poor posture – some directly identifiable, others less so. While pathological conditions (such as a congenital malformations) or external forces (unlevel shoes, for instance) can be a cause, most postural deficits can be traced to repetitive micro-traumas. Almost all healthy children around the age of 5, before beginning schooling, have no readily-identifiable postural abnormalities; at the end, almost all of them do.1 Similarly, scoliosis seldom has a direct cause, but in some populations is so prevalent as to be considered practically a normal phenomenon.2 Understanding both scoliosis and poor posture as mal-adaptations to imposed demands leads us to search for similarities between the two, and may provide helpful clues for postural rehab.
Axial loading of the spine: it’s all in your head!
One of the main drivers of adaptation is the innate desire of our nervous system to expend as little resources as possible on tasks such as balance, posture, and co-ordination; in essence, to operate in a “minimum-energy state.” Understanding how to use this natural tendency towards energy conservation to your advantage is a key factor in postural rehab.
Spinal imbalances frequently arise as a consequence of the body’s attempt to integrate the primary righting reflex – our vision – with the proprioceptive feedback from the rest of the body and maintain erect bipedalism. The unique mechanics of the fully upright human spine play a decisive role in the pathogenesis of scoliosis.3 While scoliosis can be induced in an animal model artificially, humans are the only species on Earth that spontaneously develop idiopathic, structural scoliosis. Human bipedalism induces forces into the spine which predispose the spine to rotate in a certain fashion; in non-scoliotic spines, there is a pre-existent pattern of rotation, similar to what is observed in idiopathic scoliosis, which is lessened when a quadrupedal-like (on hands-and-knees) position is adopted.4
Compressively loading the spine exacerbates spinal curvature.5 Renee Cailliet, MD stated that for every inch of forward head translation, ten pounds of compressive loading are applied to the spine.6 Positive sagittal imbalance predicts health-related quality of life in adult scoliosis patients,7 and forward head posture (FHP) is a common clinical finding in adolescent scoliosis patients that can lead to a flexion or “librarian”-type posture.8
The typical scoliosis patient exhibits right head tilt; when the visual righting reflex establishes its dominance, a right high shoulder manifests. This chain reaction continues in the form of a left low hip and left weight-bearing foot behind the right one. Whether the righting reflex is a cause or effect of the scoliosis, the end result is that it reinforces the spinal deformity. To correct postural abnormalities, begin by examining how the righting reflex of the eyes affects them.
Self-correction of posture versus Innate Correction

Without proper instruction, many strategies employed by people to correct their posture actually have a detrimental effect. Research suggests verbal commands to “stand up straight!” are insufficient to retrain children’s postural habits, and may cause a worsening of the thoracic kyphosis, with little to no effect on the lumbar lordosis.9 This information is especially poignant to the parents of children with scoliosis; thoracic lordosis is a predominant component of the deformity,10,11 and this research suggests that this is aggravated when the parents instruct their children to ‘straighten up.’
This phenomenon is not isolated to the sagittal plane, either; the “pathological pattern of incorrect posture” involved in scoliosis leads to alterations in body weight distribution (e.g., bilateral weight scales).12 When patients were instructed to equalize their weight distribution, the deformity worsened in subjects with scoliosis, and non-scoliosis patients developed spinal asymmetries. An active attempt on the part of the untrained patient to “self-correct” their posture appears to lead to further sagittal and coronal imbalances.
The patient’s posture may be changed passively through a brace; however, the obvious detriment is that any corrective benefit is lost after a sustained period outside of the brace. This is exemplified in scoliosis, where this loss of correction has prompted many researchers to suggest an exercising during weaning to prevent this.13 For non-scoliotic patients, there are numerous braces on the market which claim to improve posture; however, very few published studies exist regarding their effectiveness, and while they may show improvement in-brace, there is no evidence that this correction is maintained out of the brace.
With immobilization, muscular atrophy and disc degeneration is accelerated.14,15 There are concerns that bracing could encourage a mild, postural scoliosis to develop into a rigid and permanent spinal deformity. Bracing is an effective short-term solution for sprains, strains, and sports injuries; however, there is insufficient evidence that bracing creates long-term postural changes, and increasing evidence that long-term immobilization has dramatic negative effects.
New research, new possibilities
If telling the patient to “stand up straight” won’t work, and bracing is not an ideal long-term solution, the question remains, what is the best method of correcting posture? Firstly, by recognizing that balance, posture, and co-ordination are regulated primarily by the cerebellum as involuntary and automatic responses. Altering posture through active muscle contraction can actually have the opposite of the intended effect. The improvements documented in a case series of 19 scoliosis patients has implications for non-scoliotic patients.16 Rather than focusing on active, patient-initiated exercises, or passive, external methods, there is a third option: re-active therapy. Have you ever observed someone carrying a heavy bag at an airport? Too much weight pulls them over, but with the right amount, they react and counter-balance for the uneven load, thereby affecting their spine and posture.
There exists a motor-sensory feedback loop between the postural regulation systems of the cerebellum and the intrinsic spinal musculature; improper processing of vestibular signals by the CNS may lead to spinal deformity, which in turn prompts the development of new neuromuscular motor control strategies.17 In scoliosis, whether it is a defect of the CNS or a purely mechanical issue that initiates the process, once the curvature is present, both biomechanical and neuromuscular forces become involved in its progression.18 This creates a “Vicious Cycle” of scoliosis progression leading to imbalanced forces, which then encourage further progression. Arresting this cyclical pathology demands recognition of all of the biomechanical, soft tissue, and neuromuscular adaptations involved – this does not apply only to the scoliotic population, but to all individuals with postural problems.
Basic principles of re-active therapy
It is imperative in re-active therapy that the patient is standing on an unstable surface, such as a foam pad or inflated disc. By first destabilizing the patient, we increase the communication that is required between the brain and the body to maintain overall balance; perturbation initiates the process of consolidation in balance-control strategies.19 Next, a patient-specific system of weights, cantilevers, and therapy glasses are combined to achieve ideal posture, or even an over-correction. The idea is primarily to work with the body’s natural righting reflexes; if the patient has a right head tilt, and through re- active therapy we can induce a left head tilt, as the eyes balance out to the horizon, we achieve a complete reversal of the physical stance of the body. This form of dynamic rehabilitation is not active therapy, as it does not require the patient to perform any form of conscious, self-directed motion.
Rather they are re-acting to the imposed demands without conscious thought. Posture should be rehabilitated in the same manner that it began to deteriorate – without conscious thought.One quick note: it is surprisingly easy to measure posture in a quantifiable manner, with the aid of inexpensive and readily available software programs. Furthermore, the accuracy of these methods has been established in the peer-reviewed literature.20 Assigning a numerical value to postural deviations greatly enhances the perceived value of care; it is one thing to tell a patient that their posture has improved, but quite another to be able to tell them that their right shoulder, which was 1.13 inches higher than their left, is now only 0.34 inches higher. These objective measurements reinforce the patient’s confidence in the effectiveness of chiropractic. As Galileo famously stated, “Measure what is measurable, and make measurable what is not so.”
Chiropractors play a vital role in public health by promoting awareness of the importance of good posture. As the general public begins to recognize the numerous correlations between posture and health – including headaches,21 spinal pain,22 depression,23 impaired respiratory function,24 and increased vulnerability to injury,25,26 to name a few – it is imperative that the chiropractic profession employs effective, validated methods of measuring and improving posture objectively. The ideal method of postural rehabilitation works with the natural reflexes of the body and simultaneously addresses all of the involved aspects – including spinal biomechanics, soft tissue deformations, and neuromuscular adaptation strategies.
Research & References
- Widhe T: Spine: posture, mobility and pain. A longitudinal study from childhood to adolescence. Eur Spine J. 2001 Apr;10(2):118-23.
- Avikainen VJ, Vaherto H: A high incidence of spinal curvature: a study of 100 young female students. Acta Orthop Scand. 1983;54:267-73.
- Kouwenhoven JW, Castelein RM: The pathogenesis of adolescent idiopathic scoliosis: review of the literature. Spine 2008 Dec 15;33(26):2898-908.
- Janssen MM, Vincken KL, Kemp B, Obradov M, de Kleuver M, Viergever MA, Castelein RM, Bartels LW: Pre-existent vertebral rotation in the human spine is influenced by body position. Eur Spine J. 2010 Oct;19(10):1728-34.
- Little JP, Izatt MT, Labrom RD, Askin GN, Adam CJ: Investigating the change in three dimensional deformity for idiopathic scoliosis using axially loaded MRI. Clin Biomech 2012 Jan 4 [Epub ahead of print]
- Caillet R: Soft Tissue Pain and Disability. Philadelphia: FA Davis Co., 1977, p. 214.
- Mac-Thiong JM, Transfeldt EE, Mehbod AA, Perra JH, Denis F, Garvey TA, Lonstein JE, Wu C, Dorman CW, Winter RB: Can c7 plumb line and gravity line predict health-related quality of life in adult scoliosis? Spine 2009 Jul 1;34(15):E519-27.
- Culbert T, Olness K: Integrative Pediatrics. Oxford University Press, 2010, p. 164.
- Stolinski L, Kotiwcki T: Self-correction of posture: assessment of the quality of the movement accomplished by non-instructed school children. Scoliosis 2012 Jan 27;7 Suppl 1:O66. [Epub ahead of print]
- Dickson RA, Lawton JO, Archer IA, Butt WP: The pathogenesis of idiopathic scoliosis. Biplanar spinal asymmetry. J Bone Joint Surg. 1984 Jan;66(1):8-15.
- Millner PA, Dickson RA: Idiopathic scoliosis: biomechanics and biology. Eur Spine J. 1996;5(6):362-73.
- Nowotny J, Brzek A, Nowotny-Czupryna O, Czupryna K, Plaszewski M: Some possibilities of correction and compensation in body posture regulation among children and youth with low degree scoliosis. Scoliosis 2012, 7(Suppl 1):O64.
- Zaina F, Negrini S, Atanasio S, Fusco C, Romano M, Negrini A: Specific exercises performed in the period of brace weaning can avoid loss of correction in adolescent idiopathic scoliosis (AIS) patients: Winner of SOSORT’s 2008 Award for Best Clinical Paper. Scoliosis 2009 Apr 7;4:8.
- Eisinger DB, Kumar R, Woodrow R: Effect of lumbar orthotics on trunk muscle strength. Am J Phys Med Rehabil. 1996;75:194-197.
- Stokes IA, McBride C, Aronsson DD, Roughley PJ: Intervertebral disc changes with angulation, compression, and reduced mobility simulating altered mechanical environment in scoliosis. Eur Spine J. 2011 Oct;20(10):1735-44.
- Morningstar MW, Woggon DA, Lawrence G: Scoliosis treatment using a combination of manipulative and rehabilitative therapy: a retrospective case series. BMC Musculoskeletal Disorders 2004 Sept 14;5:32.
- Burwell RG, Dangerfield PH, Freeman BJ: Etiologic theories of idiopathic scoliosis. Somatic nervous system and the NOTOM escalator concept as one component in the pathogenesis of adolescent idiopathic scoliosis. Stud Health Tech Inform. 2008;140:208-17.
- Veldhuizen AG, Wever DJ, Webb PJ: The aetiology of idiopathic scoliosis: biomechanical and neuromuscular factors. Eur Spine J 2000 Jun;9(3):178-84.
- Tjernstrom F, Fransson PA, Hafstrom A, Magnusson M: Adaptation of postural control to perturbations – a process that initiates long-term motor memory. Gait Posture 2002, 15:75-82.
- Brink Y, Louw Q, Grimmer-Somers K: The quality of evidence of psychometric properties of three-dimensional spinal posture-measuring instruments. BMC Musculoskeletal Disorders 2011, 12:93.
- Lennon J, Shealy N, Cady RK, Matta W, Cox R, Simpson WF: Postural and respiratory modulation of autonomic function, pain, and health. Am J Pain Manag. 1994;4:36-39.
- Mieke D, Barbara C, Pascal C, Guy V, Greet C, Roseline D, Lieven D: Sagittal standing posture and its association with spinal pain: a school-based epidemiological study of 1196 Flemish adolescents before age at peak height velocity. Spine 2011 Nov 19. [Epub ahead of print]
- Canales JZ, Cordas TA, Fiquer JT, Cavalcante AF, Moreno RA: Posture and body image in individuals with major depressive disorder: a controlled study. Rev Bras Psiquiatr. 2010 Dec;32(4):375-80.
- Huggare JA, Laine-Alava MT. Nasorespiratory function and head posture. Am J Orthod Dentofacial Orthop. 1997;112(5):507-11.
- Stemper BD, Yoganandan N, Pintar FA: Effects of abnormal posture on capsular ligament elongations in a computational model subjected to whiplash loading. J Biomech. 2005 Jun; 38(6) 1313-23.
- Oktenoğlu T, Ozer AF, Ferrara LA, Andalkar N, Sarioğlu AC, Benzel EC: Effects of cervical spine posture on axial load bearing ability: a biomechanical study. J Neurosurg. 2001 Jan;94 (1 Suppl) 108-14.
Dr. Dennis Woggon is the Founder of the CLEAR Scoliosis Institute, and also founded the CLEAR Scoliosis Treatment and Research Clinic. He can be contacted at [email protected].
Dr. A. Joshua Woggon, a 2010 Graduate of Parker College, is the Associate Director of the CLEAR Scoliosis Treatment and Research Clinic in Dallas, Texas. He can be contacted at [email protected], www.clear-institute.org.
![]()

 When I was able to return to my office, an infection had left my lumbar spine in such bad shape that most activities were painful and impossible to perform. In addition, my colleague of many years decided to move on with his own practice, and I realized that my business was finished. I reluctantly wrote a letter thanking my patients for 34 years of support and assuring them that their records would be available and ready to be transferred to the provider of their choice. As I contemplated my future, my father, Dr. Burl Pettibon, came to me with an idea he was working on for a decompression system. The system utilizes simultaneous cervical and lumbar traction combined with whole body vibration and an exercise protocol. Although my practice was finished, I was able to temporarily interact with patients in a research capacity. I also had an opportunity to find out if subluxation configurations could not only be corrected but also be maintained without the typical high-velocity, low-amplitude spinal manipulation.
When I was able to return to my office, an infection had left my lumbar spine in such bad shape that most activities were painful and impossible to perform. In addition, my colleague of many years decided to move on with his own practice, and I realized that my business was finished. I reluctantly wrote a letter thanking my patients for 34 years of support and assuring them that their records would be available and ready to be transferred to the provider of their choice. As I contemplated my future, my father, Dr. Burl Pettibon, came to me with an idea he was working on for a decompression system. The system utilizes simultaneous cervical and lumbar traction combined with whole body vibration and an exercise protocol. Although my practice was finished, I was able to temporarily interact with patients in a research capacity. I also had an opportunity to find out if subluxation configurations could not only be corrected but also be maintained without the typical high-velocity, low-amplitude spinal manipulation. Presenting Complaints:
Presenting Complaints: Presenting Complaints:
Presenting Complaints: The Retail Clerk (51-year old female)
The Retail Clerk (51-year old female)
 Posture is not a conscious decision but a subconscious relationship with our environment.
Posture is not a conscious decision but a subconscious relationship with our environment.
 Several years ago I was practicing in the Houston area. My daughter attended a private school just north of Houston that had a nationally ranked basketball program. I was a pretty involved parent, and it doesn’t take long for the school to discover which parents have useful skills. I was happy to help whenever I could, to keep the school’s athletes in top form, but more importantly to help the young people get the most possible enjoyment from their high school years.
Several years ago I was practicing in the Houston area. My daughter attended a private school just north of Houston that had a nationally ranked basketball program. I was a pretty involved parent, and it doesn’t take long for the school to discover which parents have useful skills. I was happy to help whenever I could, to keep the school’s athletes in top form, but more importantly to help the young people get the most possible enjoyment from their high school years.
 First, as a chiropractor I must be able to get positive results for my patients concerning both their goals and mine. The patients must feel that I am there “for them” and that their goals are the most important in our relationship.
First, as a chiropractor I must be able to get positive results for my patients concerning both their goals and mine. The patients must feel that I am there “for them” and that their goals are the most important in our relationship.
 Posture is a classic example of a condition which lacks a medical label to apply to it, but nonetheless has a dramatic effect upon health. Due to the fact that “poor posture” is not recognized as a medical condition, very little standardized research can be performed upon it, and this makes it difficult to understand its etiopathogenesis and the ideal methods to combat it. However, there are few diseases which have as strong an association with posture as scoliosis, and ongoing research on scoliosis may shed some light on the best strategies for patients suffering from imbalanced posture.
Posture is a classic example of a condition which lacks a medical label to apply to it, but nonetheless has a dramatic effect upon health. Due to the fact that “poor posture” is not recognized as a medical condition, very little standardized research can be performed upon it, and this makes it difficult to understand its etiopathogenesis and the ideal methods to combat it. However, there are few diseases which have as strong an association with posture as scoliosis, and ongoing research on scoliosis may shed some light on the best strategies for patients suffering from imbalanced posture. Without proper instruction, many strategies employed by people to correct their posture actually have a detrimental effect. Research suggests verbal commands to “stand up straight!” are insufficient to retrain children’s postural habits, and may cause a worsening of the thoracic kyphosis, with little to no effect on the lumbar lordosis.9 This information is especially poignant to the parents of children with scoliosis; thoracic lordosis is a predominant component of the deformity,10,11 and this research suggests that this is aggravated when the parents instruct their children to ‘straighten up.’
Without proper instruction, many strategies employed by people to correct their posture actually have a detrimental effect. Research suggests verbal commands to “stand up straight!” are insufficient to retrain children’s postural habits, and may cause a worsening of the thoracic kyphosis, with little to no effect on the lumbar lordosis.9 This information is especially poignant to the parents of children with scoliosis; thoracic lordosis is a predominant component of the deformity,10,11 and this research suggests that this is aggravated when the parents instruct their children to ‘straighten up.’ 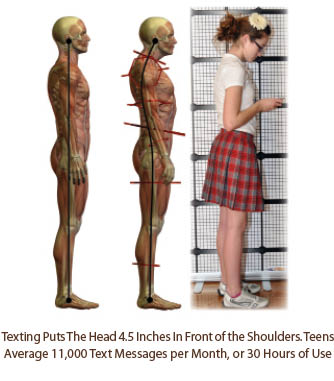
 Consider the conclusions from two recent studies:
Consider the conclusions from two recent studies: While developing a new posture grid for school posture exams, the author placed a typical middle school youth in front of the grid and asked the youth to send out a text. It was discovered that the head was placed in a position 4.5” in front of the shoulders and placed the shoulder joints in internal rotation. The typical youth can text up to 30 hours per month.
While developing a new posture grid for school posture exams, the author placed a typical middle school youth in front of the grid and asked the youth to send out a text. It was discovered that the head was placed in a position 4.5” in front of the shoulders and placed the shoulder joints in internal rotation. The typical youth can text up to 30 hours per month.
 :dropcap_open:F:dropcap_close:ascial therapy has become a very popular technique over the past several years. Fascia is the term applied to all of the connective tissues fibers and glue of the human body. Many tools to perform fascial therapy have gained popularity amongst Chiropractors, physiotherapists, personal trainers, and massage therapists. In addition to our hands (ART, myofascial release), key instruments used for fascial therapy are Sound Assisted Soft Tissue Mobilization (SASTM) tools, Graston tools and the Deep Muscle Stimulator (DMS).
:dropcap_open:F:dropcap_close:ascial therapy has become a very popular technique over the past several years. Fascia is the term applied to all of the connective tissues fibers and glue of the human body. Many tools to perform fascial therapy have gained popularity amongst Chiropractors, physiotherapists, personal trainers, and massage therapists. In addition to our hands (ART, myofascial release), key instruments used for fascial therapy are Sound Assisted Soft Tissue Mobilization (SASTM) tools, Graston tools and the Deep Muscle Stimulator (DMS).
 Now that we are in the middle of summer, many of our patients ask us about outdoor activities and what they should do and not do. We usually instruct our patients to warm up a little with some walking and some simple range of motion stretches involving the major muscle groups before starting their outdoor projects. For our more sedimentary patients, we may even tell them to take time every 15 minutes to stand up and stretch after they have been in one specific posture for a period of time. For many people, spring and summer bring on a new resolution of getting out and exercising more frequently. This commonly is in the form of walking, jogging, and for some, running.
Now that we are in the middle of summer, many of our patients ask us about outdoor activities and what they should do and not do. We usually instruct our patients to warm up a little with some walking and some simple range of motion stretches involving the major muscle groups before starting their outdoor projects. For our more sedimentary patients, we may even tell them to take time every 15 minutes to stand up and stretch after they have been in one specific posture for a period of time. For many people, spring and summer bring on a new resolution of getting out and exercising more frequently. This commonly is in the form of walking, jogging, and for some, running.
 :dropcap_open:O:dropcap_close:steoporosis and obesity are important health concerns in the United States. Whole-body Vibration (WBV) therapy has the potential to make a significant impact upon musculoskeletal health and wellness in the coming decade.1,2 It also has the potential of causing significant musculoskeletal harm, and becoming a significant source of doctor liability, if improperly applied.
:dropcap_open:O:dropcap_close:steoporosis and obesity are important health concerns in the United States. Whole-body Vibration (WBV) therapy has the potential to make a significant impact upon musculoskeletal health and wellness in the coming decade.1,2 It also has the potential of causing significant musculoskeletal harm, and becoming a significant source of doctor liability, if improperly applied.