Pre-existing Injuries Increase Bodily Injury
by Dr. William J. Owens, D.C., D.A.A.M.L.P.
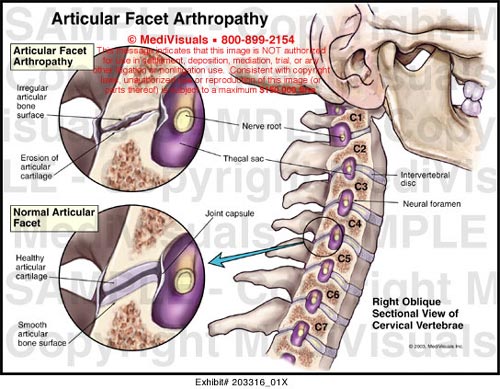
In practice, there are many challenges to overcome when rendering a proper diagnosis, prognosis and treatment plan. None is more challenging than establishing causal relationship in patients that have pre-existing degenerative changes in their spine and surrounding tissues. Degenerative changes include intervertebral disc herniation (one or more levels), surgical fusion (one or more levels), spondylosis and hypertrophy of the ligamentum flavum, to name a few. How do pre-existing changes affect the forces of trauma? Does this put the body at increased risk?
Until recently, there has been little information to be found in peer reviewed, Medline indexed journals addressing this frustrating clinical presentation. In order to properly protect the patient and diagnose what is truly related to the traumatic event, we can look to a very recent publication, Defining the “older” crash victim: The relationship between age and serious injury in motor vehicle crashes, Newgard, Craig 2008. This manuscript was published in Accident Analysis & Prevention 40 (2008) 1498-1505.
Accident Analysis & Prevention provides wide coverage of the general areas relating to accidental injury and damage, including the pre-injury and immediate post-injury phases. Published papers deal with medical, legal, economic, educational, behavioral, theoretical or empirical aspects of transportation accidents, as well as with accidents at other sites. Selected topics within the scope of the Journal may include studies of human, environmental and vehicular factors influencing the occurrence; type and severity of accidents and injury; the design, implementation and evaluation of countermeasures; biomechanics of impact and human tolerance limits to injury; modeling and statistical analysis of accident data; policy, planning and decision-making in safety.
This paper looked to establish a baseline age in which trauma victims can expect to be injured more severely in a motor vehicle accident. Is there a distinct relationship between the age of the occupant and the severity of the injury? This study included 100,156 adult front seat passengers, of which 14,128 were seriously injured. While mortality in drivers seems to be a major focus in research, serious injury continues to be a serious issue in morbidity and mortality, especially in the elder population. The author writes, “One question that arises from these results is why age is such an important predictor of injury. Age is a surrogate for increasing rates of comorbid conditions (e.g., cardiovascular disease, diabetes, pulmonary disease, renal dysfunction), any of which may result in increased morbidity and mortality after injury.” (Newgard 2008, p1503). The paper goes on to say, “However, the assessment of serious injury as the outcome may be less affected by the presence of comorbid conditions and more reflective of the inherent physical intolerance to the biomechanical stress of traumatic events. That is, as occupants age, they become inherently more fragile and less tolerant to the multitude of forces involved in a MVC.” (Newgard 2008, p1503). What the author actually demonstrated in this article is that chronological age has less to do with injury severity than physiological age. We all know patients that age gracefully and those that unfortunately do not. When assessing the trauma patient, physiologic age will have an important influence on diagnosis and prognosis of the injury. Factors that are influenced by physiologic age include:
1. Reduced Tissue Elasticity—This factor has a profound impact on how forces are distributed during a traumatic event. A flexible spine is more resilient than a stiff spine. This also includes surgical or developmental fusion.
2. Decreased Bone Density—The more brittle the bone matrix, the more susceptible the victim is to compression fractures and acute Schmorl’s Nodes. Bone mass can be affected by early entry into menopause, smoking, lack of weight bearing exercises and some metabolic/hormonal disorders.
3. Damaged Vascular Beds—Ligament and tendinous structures have limited vascularization, which prolongs healing time and increases the risk of re-injury. With increased physiologic age, these conditions get worse. Examples include cardiovascular disease, pulmonary disease, smoking and diabetes mellitus. Patients with vascular claudication may be at a much higher risk as well.

When evaluating patients for potential causally related injuries, the physiologic age of the victim is a very important concept to address. This should not only be considered during the evaluation process, but it also needs to be articulated to the patient. This not only helps to justify care but will also increase patient compliance.
Each issue, a clinical topic will be provided by Dr. William J. Owens of the American Academy of Medical Legal Professionals (AAMLP), which is a national non-profit organization comprised of doctors and lawyers. The purpose of the organization is to provide its members with current research in trauma and spinal-related topics to keep the professional on the cutting edge of healthcare. Members may also sit for a Diplomate examination and be conferred a DAAMLP. The organization also offers support to the individual member’s practice. To learn more, go to www.aamlp.org or call 1-716-228-3847.
The above review is provided for educational purposes only. It is not designed or intended to reproduce or replace the authors’ work. Readers are encouraged to obtain full licensed versions of the article as determined by Copyright Law. For information on how to obtain a licensed copy, please contact the Academy and Dr. Owens directly at [email protected].