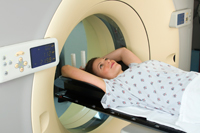
Mrs. Jones enters your office complaining of leg pain or arm pain and you perform a clinical examination which reveals a radicular component, or worse, a myelopathic component. At the end of the examination, you order and take X-rays and, upon your clinical conclusion, do a diagnostic work-up, as you aren’t sure of the etiology of the neurological involvement.
You have 3 avenues for communication with your patient:
• Choice #1: You tell the patient that you are going to embark on a conservative course of care, with gentle adjustments and, at the end of 6-8 weeks, should the problem persist, you will consider an MRI.
• Choice #2: You tell your patient that you aren’t really sure of what’s going on; however, you want to embark on a course of delivering high velocity thrusts into his/her spine. If you’ve guessed right, he/she will be just fine. If you’ve guessed wrong, then there is a chance that you can hurt him/her badly, possibly causing permanent neurological problems that will necessitate surgery or worse…. But, not to worry, because you are a really good guesser…. So let’s get going!!!!!!
• Choice #3: You tell the patient that you really aren’t sure of what’s going on; so, before you proceed with care, you are ordering an immediate MRI to get an accurate diagnosis, create an accurate prognosis and then design the treatment plan.

What is the difference between scenarios #1 and #2? Nothing, as they both say the same thing and #1 is eloquent nonsense while, in scenario #2, the sobering truth is told. In speaking across the country to doctors and members of chiropractic state boards, the consensus of the rule is consistent: IF YOU DO NOT KNOW, YOU DO NOT TOUCH.
Somewhere along the way, the insurance companies hired some slick lawyers to go to court and argue that MRI’s shouldn’t be paid for if there isn’t 6-8 weeks of conservative care prior to the MRI being performed and the only time an MRI should be considered prior to the 6-8 week waiting period is if it is urgent. Then it exclusively is performed in an emergency room. When that reimbursement ruling first came down 10+ years ago in New York, I contacted both the Secretary for Chiropractic and the Secretary for Medicine (for confirmation) in the New York State Department of Education; the answer was clear and is consistent nationally. “If you think there is a neurological problem of the root or cord and there remains a diagnostic dilemma as to etiology, you are bound to use every means available to conclusively diagnose your patient. That includes an MRI, regardless of the pressure of the insurance companies.” They went on to further state, “If you do not do the MRI and your patient gets hurt because of underlying pathology, you stand a good chance of losing your license.”
Do not lose sight of the fact that denying MRI’s is a big business for insurance companies and you are often a willing accomplice to their business plan at both your own peril and that of your patients. We do not answer to the insurance companies or the courts. Our covenant is with our state licensure boards that are charged with protecting the people of our state. You are bound to follow those standards.
I have had a simple rule for decades; if there is a radiculopathic or myelopathic involvement, I will always order an MRI prior to adjusting the patient. These are as a result of a space occupying lesion and I need to be certain of what that lesion is. You do too. If I don’t know, I don’t touch.
Radiculopathy is not a specific condition, but rather a description of a problem in which one or more nerves are affected and do not work properly (a neuropathy). The emphasis is on the nerve root (Radix=”root”). This can result in pain (radicular pain), weakness, numbness, or difficulty controlling specific muscles.
In a radiculopathy, the problem is at or near the root of the nerve, along the spine. However, the pain or other symptoms may manifest in an extremity through a process called referred pain. For example, a nerve root impingement in the neck can produce pain and weakness in the forearm. Likewise, an impingement in the lower back or lumbar-sacral spine can be manifested with symptoms in the foot.1
Myelopathy refers to pathology of the spinal cord. When due to trauma, it is known as spinal cord injury. When inflammatory, it is known as myelitis.2
In addition, myelopathy is a compression of the spinal cord with ensuing neurological deficit distal to the level of lesion. Aggressive chiropractic care is indicated in almost every instance. However, in that small percentage of patients who fall into the latter category, you will be grateful you ordered MRI’s and practiced with certainty. Your goal is simple; create an accurate diagnosis, prognosis and treatment plan prior to delivering your treatment.
To take it a step further, you must learn to interpret your own MRI’s, as general radiologists, having only 6 weeks as a rule in spinal MRI training, have an error rate upwards of 40%. Be in full control of your patients’ care and your practice and win by being the best-of-the-best.
Dr. Mark Studin is a consultant and educator. He teaches how, through clinical excellence, to build PI practices and can be found at www.teachchiros.com. He is also the creator of the US Chiropractic Directory that hosts the world’s first CV builder for chiropractors and offers that for free to doctors of chiropractic and can be found at www.USchirodirectory.com.
References
1. Wikipedia. (n.d). Retrieved from http://en.wikipedia.org/wiki/Radiculopathy.
2. Wikipedia. (nd.). Retrieved from http://en.wikipedia.org/wiki/Myelopathy.