Increased thoracic kyphosis is associated with osteoporosis and results in a reduced quality of life (QOL). It is also associated with alteration of postural balance, resulting in increased risk of falling. Falls in the geriatric population are associated with increased incidence of fracture.2 Among older adults (those 65 or older), falls are one of the leading causes of injury and death. They are also the most common cause of nonfatal injuries and hospital admissions for trauma. In 2010, 2.3 million nonfatal fall injuries among older adults were treated in emergency departments and more than 662,000 of these patients were hospitalized.3
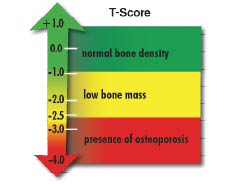
Increased thoracic kyphosis is associated with osteoporosis and results in a reduced quality of life (QOL). It is also associated with alteration of postural balance, resulting in increased risk of falling. Falls in the geriatric population are associated with increased incidence of fracture.2 Among older adults (those 65 or older), falls are one of the leading causes of injury and death. They are also the most common cause of nonfatal injuries and hospital admissions for trauma. In 2010, 2.3 million nonfatal fall injuries among older adults were treated in emergency departments and more than 662,000 of these patients were hospitalized.3 - A T-score within 1 standard deviation (SD) (+1 or -1) of the young adult mean indicates normal bone density.
- A T-score of 1 to 2.5 SD below the young adult mean (-1 to -2.5 SD) indicates low bone mass.
- A T-score of 2.5 SD or more below the young adult mean (more than -2.5 SD) indicates the presence of osteoporosis.
- In general, the risk for bone fracture doubles with every SD below normal. Thus, a person with a BMD of 1 SD below normal (T-score of -1) has twice the risk for bone fracture as a person with a normal BMD. A person with a T-score of -2 has four times the risk for bone fracture as a person with a normal BMD. When this information is known, people with a high risk for bone fracture can be treated with the goal of preventing future fractures.
- Severe osteoporosis is defined as having a bone density that is more than 2.5 SD below the young adult mean with one or more past fractures due to osteoporosis.
- The Z-score is your BMD as compared to an age-matched norm. Z-scores are calculated in the same way, but the comparisons are made to someone of the same age, sex, race, height, and weight.5
According to the National Osteoporosis Foundation, women who are taking an osteoporosis medication should have a DEXA scan every two years.6 There is not, however, a firm consensus on this point, as in extreme cases, or very high-risk cases, more frequent testing is advised. Many insurance companies and HMOs resist testing patients until age 65. In light of the serious impact of this disease on patients, and the trend toward a more sedentary lifestyle in industrialized nations, testing should be done much earlier. A proactive approach could represent actual preventative healthcare. Furthermore, the initial radiographic screening done by most chiropractors is an important early detection tool to assess bone health and structural integrity.
Due to many factors in the healthcare marketplace of 2013, chiropractors are often the de facto family physician for many individuals, and represent a direct portal of entry into the healthcare system. Chiropractors should be ever mindful of the nature of each patient’s macro- and microstructure in order to deliver safe, superior care and management of each patient’s musculoskeletal system. In addition, chiropractors should fully evaluate the variety of clinical approaches to treating osteopenia, osteoporosis, and abnormal posture in order to insure the delivery of the highest standard of patient care.
There is broad consensus in the literature that weight-bearing activities produce healthier bone. The fact is that bone remodels to stress imposed (Wolf’s law). The interrelationship of these two natural processes has a profound impact upon the human frame. Gravity can be friend or foe, depending upon the loading of the skeleton. Gross alignment or malalignment of the skull, thorax, and pelvis have a profound impact upon the vertebral motor units, long bones, and the bones of the ankle and foot. Attention to postural alignment and, therefore, structural loading of the spine and articulated skeleton is essential to thorough patient care.
Sustained abnormal posture produces microstructural changes to the vertebrae, and eventually, alterations in the architecture of the spine. For example, the end stage of forward head posture and concomitant hyperkyphosis is an ever-worsening breakdown of the thoracic spine, often resulting in extreme distortion of the torso and a perpetual progression of forward head and torso weight bearing. Absent a walker, patients are unable to maintain upright posture. Further deterioration often leads to a fall, and the resulting grave consequences as described earlier, or life confined to a wheel chair. Enlisting gravitational force as a “friend” instead involves specific structured exercise, ergonomic considerations, and in instances of restricted spinal mobility, manipulative procedures to improve mobility and improve the overall weight-bearing posture.
Exercise that is either of low intensity or does not involve skeletal loading, primarily or secondarily as described earlier, is largely ineffective in countering bone loss or improving bone density in postmenopausal individuals.10 In this author’s opinion, based upon experience, low-intensity muscular loading is also ineffective in altering global postural weight bearing and in improving core strength. In order to improve posture and optimize sagittal balance, optimized maximal loading of the motor units and related musculotendinous tissues must be consistently employed.
Eccentric exercise has many benefits over either concentric or isometric exercise. The primary benefit is the fact that the metabolic demand of eccentric exercise is less than other forms of training. Also, in light of the fact that muscles are from 1 to 1.5 times stronger in eccentric contraction than concentric contraction, the potential for safe maximum loading in the performance of eccentric loading is tremendous.
In approaching the patient with abnormal posture and, therefore, altered weight bearing, further complicated by muscular deconditioning, the physician must design long bone and skeletal stimulation loading sufficient to induce desired bone density increases, while safely loading the musculoskeletal system to minimize negative consequences.
One of the most advanced methods for safely loading the musculoskeletal system involves whole body vibration (WBV). There are a number of vendors that supply these products, PowerPlate® and WAVE® Exercise are two I am familiar with that provide a wealth of information on their websites about WBV training.
In some instances, highly supervised weight training using conventional equipment can be employed. However, the risk is high for injury and the learning curve for performing most exercises or maneuvers is demanding. Static/isometric loading in optimized biomechanical positions and incorporating coaching to insure maximum possible recruitment is advisable. Specific equipment to achieve desirable loading with a less demanding learning curve and reduced risk of injury is available from Performance Health Systems, Inc., which produces a commercial product known as bioDensity®.
The decision to address microstructural challenges as well as gross postural distortions or macrostructural dysfunction is one each practicing clinician must address. This author has witnessed the tremendous benefits of integrating this comprehensive approach in clinical practice and what it means to patient’s lives.
References:
1. International Osteoporosis Foundation 2011
2. Influence of Sagittal Balance and Physical Ability Associated with Exercise On Quality of Life in Middle Aged and Elderly People Arch Osteoporos, 2011 vol. 6 (1-2) pp 13-20
3. Hornbrook MC, Stevens VJ, Wingfield DJ, Hollis JF, Greenlick MR, Ory MG. Preventing falls among community–dwelling older persons: results from a randomized trial. The Gerontologist 1994:34(1):16–23.
4. “Inter-examinar Reliabilty of the Right-Handed Cartesian Orthogonal Coordinate System for Use of Listing Postural Distortions” Bradbury and McVeigh Logan College of Chiropractic- Senior Research 1999-Dec-10
5. World Health Organization 2012
6. National Osteoporosis Foundation 2012
7. BStrong4Life® Protocol 2009-2013 Scott J. Heun, DC, CCSP, Perry Cammisa, DC
8. Archives of Physical Medicine and Rehabilitation. 1984 Oct; 65(10):593-6.
9. J Manipulative Physiol Ther. 1996 Jul-Aug;19(6):398-405. A normal sagittal spinal configuration: a desirable clinical outcome. Harrison DD, Troyanovich SJ, Harrison DE, Janik TJ, Murphy DJ.
Eur Spine J. 2002 Jun;11(3):287-93. Epub 2001 Nov 1. How do anterior/posterior translations of the thoracic cage affect the sagittal lumbar spine, pelvic tilt, and thoracic kyphosis? Harrison DE, Cailliet R, Harrison DD, Janik TJ.
Eur Spine J. 2011 September; 20(Suppl 5): 699–703. Published online 2011 August 3. doi: 10.1007/s00586-011-1938-8 PMCID: PMC3175932
Sagittal imbalance cascade for simple degenerative spine and consequences: algorithm of decision for appropriate treatment J. C. Le Huec,corresponding author1 S. Charosky,2,4 C. Barrey,3 J. Rigal,1 and S. Aunoble1
10. Mayo Clin Proc. 1989 Jul; 64(7): 762-9.Efficacy of non-loading exercises in prevention of vertebral bone loss in postmenopausal women: a controlled trial. Sinaki M, Wahner HW, Offord KP, Hodgson SF.
Dr. Scott Heun is a practicing chiropractor in Napa, CA with over 30 years of clinical experience. He is also the co-founder of B•Strong4Life® www.bstrong4life.com a revolutionary company dedicated to improving core strength, balance and bone health using a proprietary system of analysis, training and patient management. In addition, he is also a sought after chiropractic advisor and mentor, specializing in patient-centered practice and doctor patient communication www.chiropracticementoring.com
Dr. Heun can be reached at [email protected]