CASE HISTORY
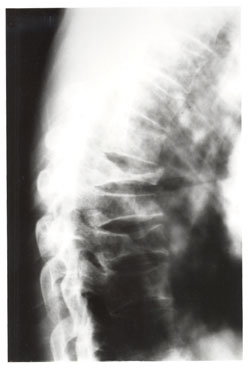
This 70-year old female lost her balance and stepped off the curb and experienced severe lower thoracic pain.
DIAGNOSIS
Observe the compression fractures of the T7, T8 and T9 vertebral bodies. Note the osteoporosis which contributed to the weakening of the vertebrae allowing these fractures to occur with minimal trauma.
GENERAL CONSIDERATIONS
Radiographic Signs of Vertebral Compression Fracture. Radiographs of optimum quality are necessary in order to adequately demonstrate these fractures. Lateral radiographs best demonstrate fracture features. Radiographic signs of vertebral compression fracture include a step defect, wedge deformity, linear zone of condensation, displaced endplate, paraspinal edema, and abdominal ileus.

The Step Defect. Since the anterior aspect of the vertebral body is under the greatest stress, the first bony injury to occur is a buckling of the anterior cortex, usually near the superior vertebral endplate. This sign is best seen on the lateral view as a sharp step-off of the anterosuperior vertebral margin along the smooth concave edge of the vertebral body. In subtle compression fractures the “step” defect may be the only radiographic sign of fracture. Anatomically, the actual step-off deformity represents the anteriorly displaced corner of the superior vertebral cortex. As the superior endplate is compressed in flexion, a sliding forward of the vertebral endplate occurs, creating this roentgen sign.
Wedge Deformity. In most compression fractures, an anterior depression of the vertebral body occurs, creating a triangular wedge shape. The posterior vertebral height remains uncompromised, differentiating a traumatic fracture from a pathologic fracture. This wedging may create angular kyphosis in the adjacent area. The superior endplate is far more often involved than the inferior endplate. Up to 30 percent or greater loss in anterior height may be required before the deformity is readily apparent on conventional lateral radiographs of the spine. Normal variant anterior wedging of 10 to 15 percent or 1-3 mm is common throughout the thoracic spine most marked at T11 – L2.
In all compression fractures there should be clear differentiation from an underlying pathology that has produced the fracture. Key features of pathologic fractures may be identified by loss of the posterior body height, pedicle, and other sites of destruction, a paraspinal mass while on MR imaging abnormal marrow can be demonstrated.
Linear White Band of Condensation (Zone of Impaction). Occasionally, a band of radiopacity may be seen just below the vertebral endplate which has been fractured. The radiopaque band represents the early site of bone impaction following a forceful flexion injury where the bones are driven together. Callus formation adds to the density of the radiopaque band later, in the healing stage of the fracture injury. This radiographic sign is striking when present; however, it is an unreliable sign, since it is not present as often as might be expected. Its presence, however, denotes a fracture of recent origin (less than two months’ duration).
Disruption in the Vertebral Endplate. A sharp disruption in the fractured vertebral endplate may be seen with spinal compression fracture. This may be difficult to perceive on plain films and tomography; CT provides the definitive means to identification. The edges of the disruption are often jagged and irregular. The superior endplate is more commonly fractured than the inferior endplate.
Paraspinal Edema. In cases of extensive trauma unilateral or bilateral paraspinal masses may occur which represent hemorrhage. These are best seen in the thoracic spine on the anteroposterior projection but may occur adjacent to the lumbar spine, creating asymmetrical densities or bulges in the psoas margins.
Abdominal Ileus. This may occur with severe spinal trauma and is a warning sign to the observer that the trauma has been severe and the likelihood of fracture is great. Abdominal ileus is seen radiographically as excessive amounts of small or large bowel gas in a slightly distended lumen. It occurs as a result of disturbance to the visceral autonomic nerves or ganglia from pain, paraspinal soft tissue injury, edema or hematoma.
Dr. Terry R. Yochum is a second generation chiropractor and a Cum Laude Graduate of National College of Chiropractic, where he subsequently completed his radiology residency. He is currently Director of the Rocky Mountain Chiropractic Radiological Center in Denver, Colorado, and Adjunct Professor of Radiology at the Southern California University of Health Sciences, as well as an instructor of skeletal radiology at the University of Colorado School of Medicine, Denver, CO. Dr. Yochum can be reached at 1-303-940-9400 or by e-mail at [email protected].
Dr. Chad J. Maola is a 1990 Magna Cum Laude Graduate of National College of Chiropractic. Dr. Maola is a Chiropractic Orthopedist and is available for post-graduate seminars. He may be reached at 1-303-690-8503 or e-mail [email protected]
REFERENCES
1. Yochum TR, Rowe LJ: Essentials of Skeletal Radiology, 3rd ed., Williams & Wilkins, Baltimore, Maryland, p. 513, 2005.