What it Means if you’re already using EHR software…and What It Means if you’re Planning to start This Year
:dropcap_open:C:dropcap_close:MS recently released its final rules for Stage 2 Meaningful Use under the American Recovery and Reinvestment Act (ARRA) and the Health Information Technology for Economic and Clinical Health (HITECH) Act.
At more than 600 pages, the rules are extremely detailed. Initial reactions are fairly positive, and it appears that CMS took into account the comments provided on the proposed rules by groups like the ACA and individual providers.
Here are 9 key takeaways from the newly released rules:
1. Requirement of Stage 2 Meaningful Use Criteria Delayed

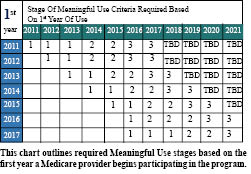
Under the proposed rules, providers were to progress to Stage 2 Meaningful Use criteria after two program years of meeting Stage 1 criteria. For example, Medicare providers who first demonstrated Meaningful Use in 2011 would need to meet Stage 2 criteria in 2013. CMS has now delayed the onset of Stage 2 criteria so that the earliest a provider would have to demonstrate Stage 2 criteria is 2014.
Note: Providers who were early demonstrators of Meaningful Use in 2011 will now meet three consecutive years of Stage 1 criteria before advancing to the Stage 2 criteria in 2014. All other providers would meet two years of Meaningful Use under the Stage 1 criteria before advancing to the Stage 2 criteria in their third year.
2. Three-month EHR Reporting Period for Stage 2 in 2014 Only
Those who completed their first year of Meaningful Use in 2011 or 2012 will only need to complete 90 days of Stage 2 Meaningful Use in 2014.
Note: This 90-day Stage 2 timeframe is ONLY for those who successfully demonstrated Meaningful Use in 2011. Then, in 2015, these providers must complete a full year of Meaningful Use. Those who begin Stage 1 Meaningful Use in 2013 will complete their first year of Stage 2 in 2015 and will be required to do so for the entire year.
This Stage 2 90-day timeframe is separate from the first-year Stage 1 90-day timeframe. All providers who begin Stage 1―no matter what the year―will only have to complete 90 days of Stage 1 Meaningful Use their first year.
It should be noted that while Meaningful Use only needs to be demonstrated for three months, you still have the full 12 months to accrue Medicare-eligible allowed submitted charges to maximize your incentive amount.
3. Stage 2 Retains Core and Menu-set Criteria Structure for Meaningful Use Objectives
Although some Stage 1 objectives were combined or eliminated, most of the Stage 1 criteria continue in Stage 2, and some menu-set criteria have become core objectives under Stage 2. For some Stage 2 objectives, the threshold percentages that providers must meet for the objective have been raised.
4. Stage 2 Criteria Consists of 20 Objectives
To demonstrate Meaningful Use under Stage 2 criteria, providers must meet 17 core objectives and three menu objectives, for a total of 20 objectives. For the menu objectives, providers must select three items from a list of six options.
5. Core and Menu-set Criteria for Stage 2 Meaningful Use
Physicians must report on most all 17 core objectives:
- Use computerized provider order entry (CPOE) for medication, laboratory and radiology orders.
- Generate and transmit permissible prescriptions electronically (eRx).
- Record demographic information.
- Record and chart changes in vital signs.
- Record smoking status for patients 13 years old or older.
- Use clinical decision support to improve performance on high-priority health conditions.
- Provide patients the ability to view online, download and transmit their health information.
- Provide clinical summaries for patients for each office visit.
- Protect electronic health information created or maintained by the Certified EHR Technology.
- Incorporate clinical lab-test results into Certified EHR Technology.
- Generate lists of patients by specific conditions to use for quality improvement, reduction of disparities, research, or outreach.
- Use clinically relevant information to identify patients who should receive reminders for preventive/follow-up care.
- Use certified EHR technology to identify patient-specific education resources.
- Perform medication reconciliation.
- Provide summary of care record for each transition of care or referral.
- Submit electronic data to immunization registries.
- Use secure electronic messaging to communicate with patients on relevant health information.
 Physicians must report on three of six Menu-Set Objectives:
Physicians must report on three of six Menu-Set Objectives:
- Submit electronic syndromic surveillance data to public health agencies.
- Record electronic notes in patient records.
- Make imaging results accessible through CEHRT.
- Record patient family health history.
- Identify and report cancer cases to a state cancer registry.
- Identify and report specific cases to a specialized registry (other than a cancer registry).
6. Clinical Quality Measures (CQMs)
All providers are required to report on CQMs in order to demonstrate Meaningful Use. Beginning in 2014, all providers—regardless of their stage of Meaningful Use—will report on CQMs in the same way.
Providers must report on nine of 64 total CQMs. In addition, all providers must select CQMs from at least three of the six key healthcare policy domains recommended by the Department of Health and Human Services’ National Quality Strategy, which include:
- Patient and Family Engagement
- Patient Safety
- Care Coordination
- Population and Public Health
- Efficient Use of Healthcare Resources
- Clinical Processes/Effectiveness
7. Patient Viewing, Downloading and Transmitting Health Information
One of the most controversial rules has to do with providing patients with the ability to view, download and transmit their health information. As such, providers must move forward with a patient portal, such as a PHR like Microsoft HealthVault or an actual portal to their EHR.
This is a significant change from Stage 1, and it will take a significant effort to educate patients and get them to initiate the exchange. In the final rule, CMS lowered the threshold to 5% and added a “broadband exclusion” for rural areas with limited broadband access.
Because secure messaging has to be initiated by patients, providers will be challenged to educate patients on the availability of secure messaging as a communication option, and it remains to be seen how feasible that will be. In short, it is feasible but may be a challenge for DCs who are less technically savvy.
8. Health Information Exchange between EHR Vendors and Organizations
With the goal of furthering interoperability, the proposed rule sought to ensure that providers were exchanging health data with users of other EHR vendor systems and with other organizations.
CMS will require providers to conduct one or more successful data-exchange tests with a “CMS designated test EHR” during the EHR-reporting period. According to CMS, the intent of that proposed rule is to foster electronic exchange outside established vendor and organization networks.
In the final rule, only one demonstration of this cross-vendor organizational capability is required. This will be a one-time test for the whole year and should be an easy criterion to perform and cross off to achieve compliance for getting the incentive.
9. Secure Messaging with Patients
One Stage 2 core objective is to use secure electronic messaging in order to communicate with patients on relevant health information. A secure message must be sent using the electronic messaging function of Certified EHR software to at least 5% of unique patients you see during the reporting period.
The Incentive: Deadlines and Rewards
If you have not yet started Meaningful Use, the most you can now receive is $39,000 (from a previous high of $44,000). But you must begin Meaningful Use by October 2013 to collect up to $39,000.
If you start after October 4, 2013 and before October 3, 2014, you can qualify for up to $24,000.
If you do not start by October 3, 2014, you will get zero dollars.
Many DCs lament that they need to make more money. Compliance with this program will take several hours of work—most of which can be performed by staff—and DCs can collect up to $39,000 per provider over the next five years, with $15,000 allowed for just 90 days of effort in 2013 for first-time meaningful users.
Ninety percent of Meaningful Use criteria can be performed by staff. More than 4,896 DCs are scheduled to complete attestation for 2012 with over 1485 already successfully paid for Meaningful Use. Most of those DCs received the maximum amount of $18,000 for their first year of Meaningful Use. This is a golden opportunity to inject more than $2 billion into our profession.
Take advantage of something all healthcare providers are implementing anyways: EHR will soon be a standard of practice. You can do it with training, determination, and simply taking your first step. Choose to do it now and get paid for it, rather than being forced to do it later with no incentive money. You can be a leader or a follower.
Steven J. Kraus, DC, DIBCN, CCSP, FASA, FICC, is Founder and CEO of Future Health, the nation’s #1 provider of chiropractic-specific EHR/practice management software. He is an acknowledged expert in Health IT, including EHR (electronic health records) and the up-to-$44,000 ARRA incentive program to implement EHR.
Dr. Kraus has served―and continues to serve―on numerous committees and boards, including:
- ACA Computer & Technology Advisory
- ACA Legislative Commission
- ACA Quality Assurance and Accountability Committee
He lectures to state associations and at industry events regarding EHR and the relationship to documentation, and he presents monthly webinars on how EHR usage will impact doctors of chiropractic. For more information, visit www.FHeConnect.com/1074 or call Toll Free 1-888-919-9919, ext. 652.
 Under the proposed rules, providers were to progress to Stage 2 Meaningful Use criteria after two program years of meeting Stage 1 criteria. For example, Medicare providers who first demonstrated Meaningful Use in 2011 would need to meet Stage 2 criteria in 2013. CMS has now delayed the onset of Stage 2 criteria so that the earliest a provider would have to demonstrate Stage 2 criteria is 2014.
Under the proposed rules, providers were to progress to Stage 2 Meaningful Use criteria after two program years of meeting Stage 1 criteria. For example, Medicare providers who first demonstrated Meaningful Use in 2011 would need to meet Stage 2 criteria in 2013. CMS has now delayed the onset of Stage 2 criteria so that the earliest a provider would have to demonstrate Stage 2 criteria is 2014.
 Physicians must report on three of six Menu-Set Objectives:
Physicians must report on three of six Menu-Set Objectives: