:dropcap_open:L:dropcap_close:ow back pain is our major cause of lost workdays and workers’ compensation claims in the United States, and heart attacks are our major cause of death. Research suggests that both problems result from the same underlying cause: the high blood cholesterol levels that result from eating the standard American diet. By helping to raise their patients’ awareness of a heart-healthy diet, chiropractors may help to reduce the patients’ risk of heart attack, as well as helping to prevent damage to the structures of the spinal column.

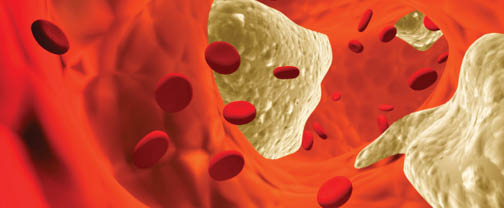
Atherosclerosis is the buildup of fatty material inside the arteries. Autopsy studies have shown that fatty streaks start to appear even in the arteries of children in Western industrialized societies.1 As the disorder progresses, these deposits may thicken and harden and eventually obstruct blood flow. When atherosclerosis restricts blood flow to the heart muscle, it produces a form of chest pain called angina. If an atherosclerotic lesion bursts and creates a blood clot, it can cause a sudden but complete blockage of blood flow through the artery. As a result, the tissue that the artery was supposed to supply with blood could die of suffocation. This area of tissue death resulting from obstruction of an artery is called an infarct. When this problem occurs in the heart muscle, it’s called myocardial infarction. When it occurs in the brain, it’s called a cerebral infarction or ischemic stroke.
Atherosclerosis is a systemic problem and can cause problems throughout the body. The atheromatous plaque tends to build up at the spots where arteries divide into smaller branches. Thus, the branching arteries that serve the lumbar spine are especially susceptible.2 The restriction of blood flow through the spinal arteries is a particular problem for the intervertebral discs, because they already have limited access to oxygen and nutrients.
The supply of oxygen and nutrients to the intervertebral discs is poor under the best of circumstances because the intervertebral discs represent the largest avascular (without blood vessels) space in the body. For an excellent review of the nutrition and metabolism of the intervertebral discs, see the doctoral dissertation of Mauno Kurunlahti.3 Any compromise of the blood circulation to the tissues surrounding the intervertebral disc results in a decrease in the provision of oxygen and nutrients to the disc and an impairment of the removal of metabolic waste products from the disc. Although the cells of the intervertebral discs can survive conditions of low oxygen tension and relatively acidic pH, their ability to produce proteoglycans under these circumstances falls off sharply. Thus, poor circulation to the tissues surrounding the intervertebral discs could initiate a process of disc degeneration.
Intervertebral discs are not supposed to have blood vessels, at least not after early childhood. Neither are they supposed to contain nerve endings. Unfortunately, if the circulation to the structures of the back is compromised badly enough, the body may try to compensate by promoting the growth of new blood vessels that invade the damaged intervertebral disc. Unfortunately, these new blood vessels can be accompanied by nerve fibers that can penetrate deep into the intervertebral disc.4 The abnormal presence of these nerve fibers may play an important role in chronic back pain. The role of atherosclerosis and abnormal innervation of intervertebral discs in causing back pain could also help to solve a mystery that has puzzled chiropractors and neurologists for years: Why it is often so difficult to pinpoint the cause of a patient’s back pain on an X-ray image.
By 1997, the Framingham study had shown a statistical relationship between low back pain and calcific lesions (a radiographic sign of advanced atherosclerosis) of the portion of the posterior abdominal aorta where the arteries that feed the lumbar spine originate.5 In 2009, a systematic review of the published literature found strong evidence to implicate atherosclerosis as a cause of low back pain. Postmortem studies showed an association between aortic atheroma and degenerative disc disease, as well as a relationship between occluded lumbar arteries and a history of low back pain. Studies of living patients found that aortic calcification was associated with low back pain and that stenosis of the lumbar arteries was associated with both degenerative disc disease and low back pain. Epidemiologic studies showed that cigarette smoking and high serum cholesterol levels had the most consistent associations with degenerative disc disease and low back pain.2
:dropcap_open:The Framingham study had shown a statistical relationship between low back pain and calcific lesions.:quoteleft_close:
The relationship between atherosclerosis and low back pain is actually good news: atherosclerosis need never exist; and, if it exists, it need never progress. By now, the evidence is overwhelming that high serum cholesterol levels are the most important risk factor for atherosclerosis. When patients keep their total cholesterol level below 150 mg/dL, atherosclerosis stops progressing and the risk of coronary artery disease becomes practically nil.6 In many patients, the atheromas actually regress.6, 7
Much of the discussion about cholesterol levels and the risk of heart disease in the United States has been distorted by an alarming fact. Only about 10% of the U.S. population currently has a total serum cholesterol of 150 mg/dL or lower. The average cholesterol levels in the U.S. population are alarmingly high, which helps to explain why heart attacks continue to be our main cause of death. In contrast, there are many other populations throughout the world where nearly everyone eats a low-fat, plant-based diet and maintains a total cholesterol level below 150 mg/dL. In those populations, coronary artery disease is rare to nonexistent.8
A low-fat (~10% of calories), plant-based diet works in three ways to reduce serum cholesterol levels.9 First, it contains zero cholesterol, which is found only in foods of animal origin. Second, a low-fat diet results in less production of cholesterol by the liver, because one of the main functions of cholesterol is to aid in the digestion of fats. Third, the fiber in plant-based foods helps to bind cholesterol in the intestine and carry it swiftly out of the body, before it can be reabsorbed and recycled.
The diet that has the best track record for preventing and reversing heart disease consists entirely of low-fat plant foods. It contains no oil or shortenings. Thanks to the increasing popularity of low-fat vegan diets, it has become easy to find cookbooks to support this kind of diet.
One of the most important clinical studies of dietary modification for reversal of heart disease is a 20-year study that was undertaken by Caldwell Esselstyn, MD, of the Cleveland Clinic. The purpose of this study was not so much to prove that heart disease could be arrested and reversed if people started eating better. That fact was already obvious because of the sharp decline in heart disease deaths in Norway during World War II. Rather, its real significance was to show that a dedicated clinician could help patients achieve this kind of success voluntarily, even when they had easy access to high-fat, high-cholesterol foods.
When it comes to preventing heart attacks and even preventing low back pain, what healthcare providers need is not more technology but better success in persuading patients to adopt a healthy lifestyle. Chiropractors have the potential to make a particularly important contribution to their patients’ health by educating their patients about how their food choices affect the health of their spine. The most important caveat is this: Patients who have any complicated medical problem may need a special nutritional consultation with a registered dietitian or diabetes educator before they make any significant change in diet. Likewise, patients who are taking prescription medication should talk to the prescriber before changing their diet. Otherwise, they could be at serious risk for adverse events such as a food-drug interaction or a sudden decrease in blood pressure or blood sugar.
Laurie Endicott Thomas has worked as a medical editor and writer for more than 20 years. She is the author of the upcoming book Where Do Gorillas Get Their Protein? Her Web site is www.gorillaprotein.com and she blogs at www.wheredogorillasgettheirprotein.blogspot.com
References
1. Stehbens WE. Relevance of hypercholesterolemia to fetal and pediatric atherosclerosis. Pediatr Pathol Mol Med 2002;21(3):259-278.
2. Kauppila LI. Atherosclerosis and disc degeneration/low-back pain–a systematic review. Eur J Vasc Endovasc Surg 2009;37(6):661-670.
2003;Available at: URL: http://herkules.oulu.fi/isbn9514270436/html/index.html.
4. Freemont AJ, Peacock TE, Goupille P, Hoyland JA, O’Brien J, Jayson MI. Nerve ingrowth into diseased intervertebral disc in chronic back pain. Lancet 1997;350(9072):178-181.
5. Kauppila LI, McAlindon T, Evans S, Wilson PW, Kiel D, Felson DT. Disc degeneration/back pain and calcification of the abdominal aorta. A 25-year follow-up study in Framingham. Spine (Phila Pa 1976 ) 1997;22(14):1642-1647.
6. Esselstyn CB, Jr. Updating a 12-year experience with arrest and reversal therapy for coronary heart disease (an overdue requiem for palliative cardiology). Am J Cardiol 1999;84(3):339-41, A8.
7. Ornish D, Scherwitz LW, Billings JH et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA 1998;280(23):2001-2007.
8. Campbell TC, Parpia B, Chen J. Diet, lifestyle, and the etiology of coronary artery disease: the Cornell China study. Am J Cardiol 1998;82(10B):18T-21T.
9. Jenkins DJ, Kendall CW, Marchie A et al. Effects of a dietary portfolio of cholesterol-lowering foods vs lovastatin on serum lipids and C-reactive protein. JAMA 2003;290(4):502-510.