:dropcap_open:I:dropcap_close:n presenting the concept of internal health—a chiropractic specialty—I have been advocating an examination approach that recognizes that muscle contraction accompanied inevitably with loss of range of motion can be caused not only by a structural problem but visceral function as well. In other words, they should not be separated when we attempt to establish the cause of chronic recurring subluxation patterns. Those of you who have been reading my articles for years know that I believe that chiropractors are the only healers that have been trained to simultaneously integrate the anatomy, physiology, and neurology involved with a patient’s symptoms before making a treatment plan. To have a treatment plan be successfully concluded, you must start by finding the cause.
That brings us to an important consideration: What tests can you perform in your office that other practitioners do not? Unfortunately, I have found that most chiropractors do not include a periodic postural screening of their patients. What better way to begin screening for muscle contraction and then find its cause? A visual inspection only takes about one minute and is one of the most effective means of patient education available to you. No expensive equipment is needed, except perhaps a full length mirror. Once postural deviations are identified and related to their symptoms, the patient can recognize when they need to return to your office—before their symptoms return.
In my two previous columns, I described how to quickly determine the structural side of weakness—be it on the left, right or, if the stress crosses over affecting the organs of the lower abdomen. In December, I discussed how to determine spinal flexibility, whether the patient can tolerate compression or decompression (traction).
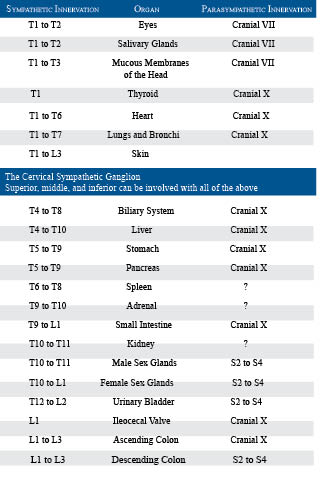
The chart on this page lists the various organs in the body. Each shares spinal innervation with a set of muscles and a specific surface area on the skin. These connections were developed during the third week of embryonic life from the ectoderm, mesoderm, and endoderm germinal layers and can provide a very accurate diagnostic system when properly employed.
Here is a suggestion that may help you to find if a visceral problem is the cause of a patient’s chronic, recurring subluxation pattern. Identify the chronic spinal subluxation and then palpate the muscles that share the innervation for contraction, soreness and pain. Most of these will be located on the anterior of the body. Next, adjust the spinal innervation. Now repalpate for the anterior contraction(s). If they are gone, the cause was structural; but, if they are still present, the cause is visceral. Who else can do that?
As you make your spinal corrections, can you name the effects that each has on the affected organ? Do you attempt to correlate the patients’ symptoms to this chart and then palpate within the affected muscles to determine if the cause of the structural subluxation or misalignment came from a visceral stress?
Once learned, this system of diagnosis adds very little time to an office call, but experience has taught me that it may very well double your referrals and income in a short period of time. That should be worth a small investment of your time. How many of the spinal innervations and autonomic effects have you committed to memory from the following list?
:dropcap_open:Successful doctors treat the cause of the problem, not the symptoms.:quoteleft_close:
Successful doctors treat the cause of the problem, not the symptoms. They are able to quickly and accurately determine the source of the patient’s stress, devise a plan of treatment, and confidently convey their findings to the patient. They specialize in helping problem cases—the ones no one else can help. They solve these cases by identifying the specific cause(s) of the patients’ symptoms that have not been identified elsewhere.
I would suggest that to enhance your practice you need the following:
- An examination that identifies the exact cause of your patient’s symptoms, be it anatomical, physiological, or neurological.
- Absolute confidence that your examination will stand the light of scientific scrutiny and will yield information quickly and accurately.
- A ceremony that both educates and inspires your patient. Ceremonies are important and you already have one. It is your office procedure.
It is my intention to continue this series by offering a series of 24 articles, one each month, each dealing with a specific visceral syndrome. I will discuss symptoms and muscle contraction patterns and related structural problems that may have become chronic because the underlying visceral dysfunction has not been identified.

 :dropcap_open:T:dropcap_close:here has been a flurry of discussion, speculation and even hard to believe health claims surrounding the supplementing of the amino acid L-arginine.
:dropcap_open:T:dropcap_close:here has been a flurry of discussion, speculation and even hard to believe health claims surrounding the supplementing of the amino acid L-arginine.
 Mental state or supplements for an improved performance?
Mental state or supplements for an improved performance?
 My New Year’s Resolution—Is Now the Time to Build or Elevate My Practice with Nutrition? A Clinical Nutritionist’s Expectation
My New Year’s Resolution—Is Now the Time to Build or Elevate My Practice with Nutrition? A Clinical Nutritionist’s Expectation Our philosophy is as a result of private counseling with patients in our clinics, and consulting with doctors nationwide. We incorporate a proprietary metabolic analyzer and software that your assistant, CA or a “wellness coach” can customize a sliding scale nutrition and exercise program based on the patient’s metabolic rate, age, height, weight, lean mass and activity level for weight loss, gain or maintenance. Our focus is to manage patient blood sugar swings effectively, without having to count carb grams, food groups or calories or providing unnecessary food restrictions. Managing blood sugars effectively usually decreases hunger, cravings, or fatigue. Our program can accommodate most patient or physician philosophies, such as Atkins, Zone, Paleolithic, Fibromyalgia or even the HCG diet protocol.
Our philosophy is as a result of private counseling with patients in our clinics, and consulting with doctors nationwide. We incorporate a proprietary metabolic analyzer and software that your assistant, CA or a “wellness coach” can customize a sliding scale nutrition and exercise program based on the patient’s metabolic rate, age, height, weight, lean mass and activity level for weight loss, gain or maintenance. Our focus is to manage patient blood sugar swings effectively, without having to count carb grams, food groups or calories or providing unnecessary food restrictions. Managing blood sugars effectively usually decreases hunger, cravings, or fatigue. Our program can accommodate most patient or physician philosophies, such as Atkins, Zone, Paleolithic, Fibromyalgia or even the HCG diet protocol.
 Howard Berg, D.C., C.C.S.P., graduated from Life Chiropractic College in 1997. He holds certifications as both a Golf Fitness Instructor and Yoga Instructor. Dr. Berg is the owner of Island Chiropractic and Wellness Center, located on St. Simons Island, Georgia.
Howard Berg, D.C., C.C.S.P., graduated from Life Chiropractic College in 1997. He holds certifications as both a Golf Fitness Instructor and Yoga Instructor. Dr. Berg is the owner of Island Chiropractic and Wellness Center, located on St. Simons Island, Georgia. Christopher Fuzy, M.S, R.D., L.D., has a Masters degree in Clinical & Sports Nutrition and undergraduate degrees in nutrition and chemistry and has implemented and trained over 700 physicians nationwide with the Lifestyle Nutrition program in the past nineteen years.For more information or a Practice Consultation, go to
Christopher Fuzy, M.S, R.D., L.D., has a Masters degree in Clinical & Sports Nutrition and undergraduate degrees in nutrition and chemistry and has implemented and trained over 700 physicians nationwide with the Lifestyle Nutrition program in the past nineteen years.For more information or a Practice Consultation, go to 

 For more information about this program, contact Dr. Cima at 1-877-627-2770 or visit
For more information about this program, contact Dr. Cima at 1-877-627-2770 or visit 



 Thiazide Diuretics
Thiazide Diuretics
