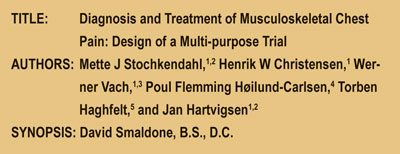
From The Abstract:
 Today, hospitals are completely overwhelmed with patients who have acute chest pain, yet no cardiac abnormalities. Often patients find themselves with nowhere to go after cardiac pain has been ruled out as a diagnosis. This study was designed to possibly determine four things: If a multi-disciplinary approach may be used to treat these patients, “To investigate the diagnostic decision making process of a chiropractor…”, to compare manual adjustment procedure vs. home care, and if chiropractic care is cost effective for this population.
Today, hospitals are completely overwhelmed with patients who have acute chest pain, yet no cardiac abnormalities. Often patients find themselves with nowhere to go after cardiac pain has been ruled out as a diagnosis. This study was designed to possibly determine four things: If a multi-disciplinary approach may be used to treat these patients, “To investigate the diagnostic decision making process of a chiropractor…”, to compare manual adjustment procedure vs. home care, and if chiropractic care is cost effective for this population.
Key Points:
1) The study had a focus population of 300 people released from care after having no “…obvious cardiac or non-cardiac disease.” Out of the 300 possible people for the study, 120 people were randomized and were separated into two populations.
2) Discussion: “This study may potentially demonstrate that a chiropractor is able to identify a subset of patients suffering from chest pain predominantly of musculoskeletal origin among patients discharged from an acute chest pain clinic with no apparent cardiac condition.” 3) Baseline measurements included:
1. “semistructured interview,
2. A general health examination, and
3. A specific manual examination.”
4) MPS(Myocardial Perfusion Scintigraphy) was used for exclusionary/inclusionary measures: “In order to evaluate the population in terms of ischemic heart disease, all patients undergo MPS within two to four weeks following baseline evaluation. Using radionuclides, the myocardial perfusion is evaluated to determine the presence of regional areas with decreased blood flow because of coronary artery disease.”
5) For the comparison of chiropractic adjustments vs. self management the RCT (Randomized Clinical Trial) measure was used. “All CTA (Cervico Thoracic Angina) positive patients (estimated 120 out of the initial 300 patients) will be included in the RCT. The aim of this part of the study is to establish the effectiveness of chiropractic treatment, including spinal manipulation versus advice to promote self-management.”
6) The study was computer randomized and blinded to the patients to chiropractic vs. home management.
7) The chiropractic treatment included: The patient must have a high velocity low amplitude adjustment and could have other soft tissues techniques in conjunction. Also, “the protocol specifies up to ten treatment sessions of approximately 20 minutes, 1–3 times per week for four weeks, or until the patient is pain free, if this occurs within less than four weeks.” The other group received 15 minutes of advice and two or three exercises to do at home.
8) Outcome measures were: The primary outcome measure was an 11point measure (0-10) scale, 6 secondary outcome measures were utilized in this experiment as well.
9) “In summary, this article presents the rationale and design of a multi-purpose study consisting of a prospective diagnostic study, and an RCT, with a cost-effectiveness study alongside the central trial. It is anticipated to be completed in 2008, at which time the results will be made available. The first part of this study may potentially demonstrate that a chiropractor is able to identify a subset of patients suffering from chest pain predominantly of musculoskeletal origin among patients dismissed from an acute chest pain clinic with no apparent cardiac condition. The long term goal is to establish whether manual palpation may be used as part of the clinical examination to screen patients allowing for improvement in referral patterns. Furthermore, knowledge about the benefits of manual treatment in patients with musculoskeletal chest pain will inform clinical decision and policy development in relation to clinical practice.”
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
 Dr. David Smaldone is a graduate of Palmer West Chiropractic College with an undergraduate in Athletic training. Dr. Smaldone has worked with thousands of Athletes in his career. He currently runs a practice in New Paltz, New York, and is an NYS licensed chiropractor. Dr Smaldone is also currently the Director of Chiropractic affairs for 123chiropractors.com.
Dr. David Smaldone is a graduate of Palmer West Chiropractic College with an undergraduate in Athletic training. Dr. Smaldone has worked with thousands of Athletes in his career. He currently runs a practice in New Paltz, New York, and is an NYS licensed chiropractor. Dr Smaldone is also currently the Director of Chiropractic affairs for 123chiropractors.com.

 Dr. Daniel J. Murphy D.C., D.A.B.C.O. graduated magna cum laude from Western States Chiropractic College in 1978. He received Diplomat status in Chiropractic Orthopedics in 1986. Since 1982, Dr. Murphy has served part-time as undergraduate faculty at Life Chiropractic College West, currently teaching classes to seniors in the management of spinal disorders. He has taught more than 2000 postgraduate continuing education seminars. Dr. Murphy is a contributing author to both editions of the book
Dr. Daniel J. Murphy D.C., D.A.B.C.O. graduated magna cum laude from Western States Chiropractic College in 1978. He received Diplomat status in Chiropractic Orthopedics in 1986. Since 1982, Dr. Murphy has served part-time as undergraduate faculty at Life Chiropractic College West, currently teaching classes to seniors in the management of spinal disorders. He has taught more than 2000 postgraduate continuing education seminars. Dr. Murphy is a contributing author to both editions of the book