:dropcap_open:O:dropcap_close:n September 8, 1965, Dorothy Dandridge, the first black American to be nominated for an Academy Award for Best Actress, was found dead. The cause was an accidental overdose of Tofranil, an anti-depressant.

Moving ahead to February 11, 2012, Whitney Houston, the world renowned singer and actress, was found dead with Xanax and alcohol in her system. Bottles of prescription drugs in her hotel room included Xanax, Valium and Ativan – all anti-depressants prescribed to treat anxiety.
Anti-depressants, anti-anxiety, and insomnia drugs truly have become “The Nightmare on Pill Street!”
In nearly 50 years of prescribing anti-depressants the results are all too frequently the same – drug addiction, mental impairment, irrational and violent behavior, panic attacks, suicide, and death. An estimated 27,000 people a year die from accidental drug overdoses in the U.S.¹ , one death every 19 minutes!
Clinical depression currently ranks second only to advanced coronary heart disease in the total number of days patients spent in the hospital or disabled at home. Pharmaceutical companies have overall yearly sales of $16 billion from anti-psychotics and $4.8 billion in sales of ADHD drugs ². As of 2005, the most recent year for which data were available, about 27 million people, or 10 percent of Americans, were taking antidepressants.³
How did the United States – whose citizens are known the world over for their outgoing self-confidence – emerge as a leading consumer of anti-depressant and anti-psychotic drugs for social anxiety? How do those of us in the profession of holistic health and natural medicine reverse this trend
Manufacturing Mental Illness
The appeal of pharmaceutical drugs is deceptively compelling. The allure that taking a pill can solve our health problems and make us feel good with little or no effort on our part is heavily promoted. In 2007, the pharmaceutical industry was estimated to be spending $4.8 BILLION dollars a year advertising prescription drugs directly to the public. The Diagnostic and Statistical Manual of Mental Disorders (DSM), published by the American Psychiatric Association, is the official manual listing psychiatric and psychological disorders. Many health professionals believe the DSM has created mental illnesses out of ordinary life experiences.
The DSM has a label and a code for most deviations from everyday behavior or passing mood swing that a person may experience4. Do you experience excessive anxiety regarding separation from people to whom you have strong emotional attachments? That’s Separation Anxiety Disorder (SAD) or code 309.21. Recurring bad dreams? That may be Nightmare Disorder, code 307.47. Then there’s the ultimate catchall for vague sadness or uneasiness, General Anxiety Disorder (GAD), code 300.02.
By perceiving ordinary life experiences as certifiable mental illness, the patient becomes treatable by psychotropic drugs and billable through insurance companies.5
Anti-depressants are no more effective than Sugar Pills!
The pharmaceutical industry claims (and advertises) that depression is caused by a shortage of serotonin — an imbalance the drug companies say can be corrected by a class of anti-depressants called Selective Serotonin Reuptake Inhibitors (SSRIs). These drugs prevent the body from metabolizing Serotonin, thereby increasing its presence in the brain.6 Prior to psychiatry’s proclamation that depression was caused by too little of the neuro-transmitter serotonin, few Americans were taking antidepressants. But by declaring that depression was caused by a serotonin imbalance, which could readily be corrected, Americans suffering from stress, insomnia and mild depression became far more receptive to taking serotonin-enhancing drugs such as Prozac, Paxil, and Zoloft.
Research, however, demonstrates that the pharmaceutical industry’s serotonin imbalance theory of depression is erroneous!
Scientists have known for quite some time that serotonin levels are not associated with depression. Research on serotonin has been clear from the very beginning that the most damaging thing that could be done to the serotonin system would be to impair one’s ability to metabolize serotonin. Yet that is exactly how SSRI antidepressants exert their effects.
A 2010 study published in the Journal of the American Medical Association (JAMA) found that anti-depressants are basically useless for the vast majority of people who take them. They were only effective on patients with very severe symptoms.7 Psychology professor Irving Kirsch, Ph.D., analyzed clinical data files from the FDA on published and unpublished trials; he found no significant differences between anti-depressant drugs and placebos. What he did find was extreme differences in side effects.8
Is there a Link connecting Anti-depressants to Violent Behavior, Suicide, and Death?
A study out of the University of Southern California in 1996 looked at a group of mutant mice in an experiment that had gone terribly wrong. These genetically engineered mice were the most violent creatures they had ever witnessed. At birth they were lacking the MAO-A enzyme which metabolizes serotonin, thus their brains were awash in this neuro-transmitter. The researchers determined this excess serotonin was the cause for the extreme violence in these mice.9
Paranoia, hallucinations, and violent behavior are all hallmark side effects of anti-depressant drugs! It now appears reasonable that anti-depressants may trigger the very symptoms they were touted to suppress. Much of the bizarre and unexplained violence in this country today may be the result of overmedication with anti-depressants and anti-psychotics.
On November 4, 2011, in Winnipeg, Canadian Judge Robert Heinrichs ruled that antidepressants like Prozac can cause children to commit murder and concluded that a 15-year-old boy was under the influence of Prozac when he fatally stabbed a close friend. The judge’s opinion was a landmark legal confirmation of the scientific fact that the newer antidepressants like Prozac, including the SSRI and SNRI anti-depressants, can cause violence and even murder.
:dropcap_open:Psychotropic drugs are a contributing cause of adverse and dangerous mental instability, sometimes causing the victims to commit suicide or murder.:quoteleft_close:
As far back as 1991, the Citizens Commission on Human Rights (CCHR) organized dozens of individuals and experts to testify before the FDA that people with no prior history of violence became homicidal and suicidal under the influence of antidepressants. To comprehend the full ramifications of these acts of violence and the concurrent use of anti-depressants, more information can be found at ssristories.com. The evidence is becoming overwhelmingly clear: Psychotropic drugs are a contributing cause of adverse and dangerous mental instability, sometimes causing the victims to commit suicide or murder.
Going Back to the Future!
Stress has always been with us. It is simply the body’s nonspecific response to any demand made upon it. Stress was programmed into primitive man to provide him with the fight or flight response necessary for his survival. But modern man is usually in situations where neither fight nor flight are viable options so his stress point – unless it can be assuaged or channeled – elevates to anxiety-producing levels. Anxiety is merely the normal response to prolonged or chronic stress. Depression is the result of being unable to handle chronic stress while insomnia can be precipitated by stress, anxiety, or depression. They are all interrelated and can be treated holistically in an effective manner.
Since the beginning of time, humans have experimented and utilized various herbs and foods for treating mood problems in an effort to maintain health. Achievements in doing so were remarkable because the plant kingdom supplies a wealth of building blocks for calmative, nervine, and muscle relaxant medicines. Unlike drugs, natural medicines address the underlying causes of stress, anxiety, depression, and insomnia while drugs attempt to treat the symptoms. Allopathic medicine is negligent in looking for the real causes of depression, such as thyroid problems, lack of exercise, a bad diet, a guilty conscience, medical problems, allergies, environmental factors, and a host of other possibilities. It’s easier and more profitable to write a prescription for an anti-depressant!
Natural Remedies for common psychological disorders
Specific herbs, minerals, and vitamins have extensive therapeutic histories and have been clinically shown to assuage and ameliorate common psychological disorders and resolve their underlying causes without subjecting the patient to synthetic drugs which are foreign and toxic to the body.
One of the most effective herbals to reduce stress – supported in the literature and by clinical research – is Rhodiola rosea which increases the body’s resistance to stress, anxiety, trauma and fatigue. Classified as an adaptogen, this herb exhibits the ability to increase resistance to a variety of chemical, biological, and physical stressors. Rhodiola also appears to regulate the body’s production of cortisol, a critical “stress hormone.10 Clinical studies have also shown Rhodiola to improve physical and mental performance, and specifically the ability to concentrate11 as well as reducing both mental and stress induced physical fatigue.12 Is this herb a viable alternative to plying our children with addictive ADHD drugs?
Hops strobiles from extract is often utilized for its calming and antispasmodic effect on the nervous system.13 Hops are fast acting. A soothing, relaxing calm may be experienced within 20-40 minutes after ingesting the herb.14
One of the most effective natural medicines to reduce anxiety – supported in the literature and by clinical research – is Inositol, a natural tranquilizer proven to help the individual by combating anxiety.15 In a 1995 double-blind study by the Ministry of Mental Health at Ben Gurion University, the efficacy of Inositol was superior to fluvoxamine, a prescription antidepressant, in patients with anxiety disorders. Patients reported side effects of nausea and fatigue with fluvoxamine. Because it is water-soluble, Inositol does not produce toxic side effects.16 Gota Kola is another neural tonic herb which has been utilized as a treatment for nervous breakdown.17
There are several medicinal herbs which have show to be effective in reducing chronic depression. One is Passiflora incarnata, which acts as a natural tranquilizer. Its analgesic effect has been demonstrated in laboratory and clinical tests.18 Passiflora works by increasing the availability of the neurotransmitter GABA (gamma-aminobutyric acid), which has a calming effect on the nerves. Again, Rhodiola rosea has been used for centuries in Russia and Scandinavia to treat both anxiety and depression.19 It has been demonstrated to effectively alleviate mild to moderate depression
The most effective natural medicine to alleviate chronic insomnia has long been an over-the-counter insomnia remedy in Germany, France, Switzerland, Belgium, and Italy. Valerian root is a sedative herb which sleep support studies clearly show improves sleep quality and sleep latency but leaves no “hangover” the next morning as is often observed with pharmaceutical sleeping aids.20 This herb has demonstrated to be especially effective when sleep disorders are the result of anxiety, nervousness, exhaustion, or hysteria.21 Another cause of sleeplessness is magnesium deficiency. Magnesium supplementation is dramatically underutilized by conventional physicians. Seventy-nine percent of adults 55 and over are not ingesting the recommended dietary allowance (RDA) of magnesium. Symptoms of a magnesium deficiency include insomnia, anxiety, hyperactivity and restlessness with constant movement, panic attacks, agoraphobia, and premenstrual irritability.22

European medical practitioners have long utilized natural medicines and herbals to regulate psychosomatic disorders. In Europe, natural medicines are prescribed like other medications and enjoy widespread scientific and medical acceptance. All German medical students, for example, must learn phyto-medicine, and approximately 80 percent of German physicians regularly use natural medications in their practice. Unfortunately, in America pharmaceutical advertising has become so pervasive and successful that psychological drugs have become a first resort, regardless of their lack of effectiveness and their draconian side effects. (The United States is one of only two countries in the world that allow pharmaceutical companies to advertise directly to the consumer.)
The public is finally becoming aware of how dangerous these anti-depressants are as more and more individuals go berserk on them! It’s beginning to exact a toll on our society. As holistic health professionals we understand that drugs are synthetic poisons and we simply cannot condone this poisoning of our citizens for profit to continue! Anti-depressant drugs are turning us into a nation of muddled, brain-addled addicts incapable of controlling our own emotions and behavior! These drugs are medically useless and physiologically dangerous. We have an obligation to speak out and educate our patients and the people we come into contact with and make them aware that superior natural alternatives to psychosomatic drugs are available. If we fail, the joke will be on us!
Reference
- Pratt L, Brody DJ, Gu Q. Antidepressant Use in Persons Aged 12 and Over: United States, 2005-2008. NCHS Data Brief. No 76. October 2011.
- IMS Health National Prescription Audit PLUS.
- Study: Number of Americans using antidepressants doubles – FierceHealthcare http://www.fiercehealthcare.com/story/study-number-americans-using-antidepressants-doubles/2009-08-05#ixzz1wO1NEbuS
- American Psychiatric Association. Practice guidelines for the treatment of patients with major depressive disorder. 2nd ed. September 2007. Accessed January 22, 2010
- Friedman, R, M.D., New England Journal of Medicine (NEJM), May 17, 2012
- Kaplan, H.I. and Sadock,B.J. Synopsis of Psychiatry, Eighth Edition, Baltimore: Williams & Wilkins. 1998
- Antidepressant Drug Effects and Depression Severity, Jay C. Fournier, MA; Robert J. DeRubeis, PhD; Steven D. Hollon, PhD; Sona Dimidjian, PhD; Jay D. Amsterdam, MD; Richard C. Shelton, MD; Jan Fawcett, MD JAMA. 2010;303(1):47-53
- Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS Med. 2008;5(2):e45
- Dr. Ann Blake Tracy of the International Coalition of Drug Awareness, testimony on September 13, 2004 before the FDA.
- Gregory S. Kelly, ND, Alternative Medicine Review 6 (3): 293–302
- Shevtsov VA, Zholus BI, Shervarly VI, et al. (Mar 2003). “A randomized trial of two different doses of Rhodiola rosea extract versus placebo and control of capacity for mental work”. Phytomedicine 10 (2-3): 95–105. PMID 12725561
- Darbinyan V, Kteyan A, Panossian A, Gabrielian E, Wikman G, Wagner H (Oct 2000). “Rhodiola rosea in stress induced fatigue—a double blind cross-over study of a standardized extract with a repeated low-dose regimen on the mental performance of healthy physicians during night duty”. Phytomedicine 7 (5): 365–71. PMID 110819
- Wohlfart, R, et al, Planta Medica, vo. 48, p. 224, 1982
- Stocker, H, Schweizer Braverei Rundschau, vol. 78, p. 80, 1967
- Cooper, AJ, Psychopharmacology, vol 61, pp 97-102, 1979
- PubMed: Journal of Clinical Psychopharmacology; Double-blind, Controlled, Crossover Trial of Inositol Versus Fluvoxamine in the Treatment of Panic Disorder
- Mowrey, DB, The Scientific Validation of Herbal Medicine, p 193, 1986
- Ambuhl, H, “Anatomische und chemische untersuchungen an Passiflor incarnata,” Dissertation Number 3830 ETH, Zurich, 1966
- Darbinyan, V.; Aslanyan, G.; Amroyan, E.; Gabrielyan, E.; Malmstroumlm, C.; Panossian, A. Clinical trial of Rhodiola rosea L. extract SHR-5 in the treatment of mild to moderate depression Nordic Journal of Psychiatry, Volume 61, Issue 5 2007 , pages 343–348.
- Leathwood, et al, Pharmacol. Biochem & Behav, vol 17, pp. 65-71, 1982
- Straube, C, Therapie der Gegenwort, vol 107, pp. 555-562, 1968
- Baker, S.M. Magnesium Deficiency in Primary Care and Preventive Medicine, Magnesium and Trace Elements, 1991-1992; 10:251-262
Galen O. Ballard is President of Titan Laboratories and directly responsible for the products division. His background includes undergraduate studies in research at the University of Denver with graduate work at the Universities of Wisconsin and Maryland. Galen may be reached toll free at 1-800-929-0945 or by email at [email protected]
 Even though you may hear reports of franchises closing in the media, the fact is that from 1971–1997, less than 5% of franchise businesses closed each year. A study conducted by the U.S. chamber of commerce found that 95% of franchises are still in business after 5 years, compared to just 47% of self-launching businesses. Buying a franchise more than doubles your chances to survive as a business owner, and by choosing the right franchise your likelihood for success can be greatly improved. So how do you choose the right franchise for you? Do you jump on the latest and fastest growing hot trends, or do you go with an older more established company everyone knows and that has a strong brand identity? Would you rather stay in your comfort zone and do something in a field you are more familiar with? Do you want a big business, small business, home based, or the chance to have multiple locations? What is the size of the market and how strong is the franchisor? The truth is, the reason most franchisors are successful comes down to just several things. First, the business model has proven to be successful and profitable and has the history and data to prove it is sustainable and not just a fad. Next, the franchisor is always striving to provide its franchisees with the best possible business tools to support them in all areas of the franchise business.
Even though you may hear reports of franchises closing in the media, the fact is that from 1971–1997, less than 5% of franchise businesses closed each year. A study conducted by the U.S. chamber of commerce found that 95% of franchises are still in business after 5 years, compared to just 47% of self-launching businesses. Buying a franchise more than doubles your chances to survive as a business owner, and by choosing the right franchise your likelihood for success can be greatly improved. So how do you choose the right franchise for you? Do you jump on the latest and fastest growing hot trends, or do you go with an older more established company everyone knows and that has a strong brand identity? Would you rather stay in your comfort zone and do something in a field you are more familiar with? Do you want a big business, small business, home based, or the chance to have multiple locations? What is the size of the market and how strong is the franchisor? The truth is, the reason most franchisors are successful comes down to just several things. First, the business model has proven to be successful and profitable and has the history and data to prove it is sustainable and not just a fad. Next, the franchisor is always striving to provide its franchisees with the best possible business tools to support them in all areas of the franchise business.


 ADHD is a neurological condition that is usually transmitted genetically. It is characterized by distractibility, impulsivity, and restlessness or hyperactivity. These symptoms are present from childhood through adulthood, and with a much greater intensity than in the everyday person, so much that they interfere with daily functioning. The Centers for Disease Control indicate that over 5 million children in the United States have ADHD*. Most children carry this condition with them into their adult years.
ADHD is a neurological condition that is usually transmitted genetically. It is characterized by distractibility, impulsivity, and restlessness or hyperactivity. These symptoms are present from childhood through adulthood, and with a much greater intensity than in the everyday person, so much that they interfere with daily functioning. The Centers for Disease Control indicate that over 5 million children in the United States have ADHD*. Most children carry this condition with them into their adult years.  The base of the SHINE model is neurological rebalancing through the application of the chiropractic adjustment. Proprioceptors located in the joints and muscles of the spine provide the largest source of information coming through the cerebellum into the brain. It is therefore crucial to ensure that there is no neural or dural tension or stress being held in the spinal structures. Adjusting the spine affects brain and nervous system function through enhancing the quality and quantity of information being conveyed into the cerebellum and subsequently the prefrontal cortex. Therefore, it is critical that the chiropractor ensures that the spine is free of all forms of tension and stress; a structured program of neurologically balancing adjustments focused on restoring neural integrity in the patient with ADHD accomplishes this goal.
The base of the SHINE model is neurological rebalancing through the application of the chiropractic adjustment. Proprioceptors located in the joints and muscles of the spine provide the largest source of information coming through the cerebellum into the brain. It is therefore crucial to ensure that there is no neural or dural tension or stress being held in the spinal structures. Adjusting the spine affects brain and nervous system function through enhancing the quality and quantity of information being conveyed into the cerebellum and subsequently the prefrontal cortex. Therefore, it is critical that the chiropractor ensures that the spine is free of all forms of tension and stress; a structured program of neurologically balancing adjustments focused on restoring neural integrity in the patient with ADHD accomplishes this goal. The SHINE for Doctors clinical care model is designed to create maximal healing and reorganization within an initial 90-day window of transformative shift. It was also created to integrate as seamlessly as possible into a chiropractic practice. The SHINE patient can be adjusted during the normal flow of patient interactions, with some coaching and monitoring of the NIMs exercise protocols and dietary changes delivered at measured intervals. Rebalancing a person’s neural and metabolic function in combination with Dr. Hallowell’s unique approach to coaching and facilitating success, provides a phenomenal platform for change within the patient with ADHD. Patients and those close to patients (parents, teachers, and coworkers) report improved school and work performance, better behavior, a happier home, better teacher, student, social, work, filial and romantic relationships, a sense of “feeling” better both emotionally and physically along with better sleep and increased ability to focus and improved self-esteem.
The SHINE for Doctors clinical care model is designed to create maximal healing and reorganization within an initial 90-day window of transformative shift. It was also created to integrate as seamlessly as possible into a chiropractic practice. The SHINE patient can be adjusted during the normal flow of patient interactions, with some coaching and monitoring of the NIMs exercise protocols and dietary changes delivered at measured intervals. Rebalancing a person’s neural and metabolic function in combination with Dr. Hallowell’s unique approach to coaching and facilitating success, provides a phenomenal platform for change within the patient with ADHD. Patients and those close to patients (parents, teachers, and coworkers) report improved school and work performance, better behavior, a happier home, better teacher, student, social, work, filial and romantic relationships, a sense of “feeling” better both emotionally and physically along with better sleep and increased ability to focus and improved self-esteem. 
 After marijuana, prescription and over-the-counter medications are the most commonly abused drugs among teenagers. These include Vicodin, Adderall, tranquilizers, cough medicine, MDMA, hallucinogens, oxycontin, and sedatives.²
After marijuana, prescription and over-the-counter medications are the most commonly abused drugs among teenagers. These include Vicodin, Adderall, tranquilizers, cough medicine, MDMA, hallucinogens, oxycontin, and sedatives.² 
 “The evidence, by itself, does not make a decision for you, but it can help support the patient care process. The full integration of these three components into clinical decisions enhances the opportunity for optimal clinical outcomes and quality of life. The practice of EBP is usually triggered by patient encounters, which generate questions about the effects of therapy, the utility of diagnostic tests, the prognosis of diseases, or the etiology of disorders. Evidence-based practice requires new skills of the clinician, including efficient literature searching, and the application of formal rules of evidence in evaluating the clinical literature” (The University of North Carolina at Chapel Hill, 2010).
“The evidence, by itself, does not make a decision for you, but it can help support the patient care process. The full integration of these three components into clinical decisions enhances the opportunity for optimal clinical outcomes and quality of life. The practice of EBP is usually triggered by patient encounters, which generate questions about the effects of therapy, the utility of diagnostic tests, the prognosis of diseases, or the etiology of disorders. Evidence-based practice requires new skills of the clinician, including efficient literature searching, and the application of formal rules of evidence in evaluating the clinical literature” (The University of North Carolina at Chapel Hill, 2010).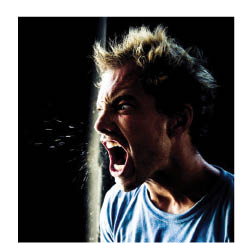
 Moving ahead to February 11, 2012, Whitney Houston, the world renowned singer and actress, was found dead with Xanax and alcohol in her system. Bottles of prescription drugs in her hotel room included Xanax, Valium and Ativan – all anti-depressants prescribed to treat anxiety.
Moving ahead to February 11, 2012, Whitney Houston, the world renowned singer and actress, was found dead with Xanax and alcohol in her system. Bottles of prescription drugs in her hotel room included Xanax, Valium and Ativan – all anti-depressants prescribed to treat anxiety. European medical practitioners have long utilized natural medicines and herbals to regulate psychosomatic disorders. In Europe, natural medicines are prescribed like other medications and enjoy widespread scientific and medical acceptance. All German medical students, for example, must learn phyto-medicine, and approximately 80 percent of German physicians regularly use natural medications in their practice. Unfortunately, in America pharmaceutical advertising has become so pervasive and successful that psychological drugs have become a first resort, regardless of their lack of effectiveness and their draconian side effects. (The United States is one of only two countries in the world that allow pharmaceutical companies to advertise directly to the consumer.)
European medical practitioners have long utilized natural medicines and herbals to regulate psychosomatic disorders. In Europe, natural medicines are prescribed like other medications and enjoy widespread scientific and medical acceptance. All German medical students, for example, must learn phyto-medicine, and approximately 80 percent of German physicians regularly use natural medications in their practice. Unfortunately, in America pharmaceutical advertising has become so pervasive and successful that psychological drugs have become a first resort, regardless of their lack of effectiveness and their draconian side effects. (The United States is one of only two countries in the world that allow pharmaceutical companies to advertise directly to the consumer.)
 The same can be said for our chiropractic practice brethren. In addition to offering a wider range of patient payment options beyond cash and checks, including credit and debit cards and e-payment, increasingly sophisticated and fully useful software solutions are automating once paper-based clinical and business applications while facilitating integration with collection agencies and clearinghouses.
The same can be said for our chiropractic practice brethren. In addition to offering a wider range of patient payment options beyond cash and checks, including credit and debit cards and e-payment, increasingly sophisticated and fully useful software solutions are automating once paper-based clinical and business applications while facilitating integration with collection agencies and clearinghouses. 
 There are distinct challenges in terms of managing cash flow and collecting patient payments for smaller professional practices with limited back-office staff to manage all the administrative processes needed to support the business.
There are distinct challenges in terms of managing cash flow and collecting patient payments for smaller professional practices with limited back-office staff to manage all the administrative processes needed to support the business. 
 Fiore in 2012 reported that accurate diagnosing was critical to the success of the chiropractic profession in order to be credible in the health care community. He also reported that many chiropractors hide behind the definition of chiropractic as the “…art, science and philosophy of locating and correcting nerve interference…” and continued on to say “This allows the chiropractic profession to have great latitude…but does not excuse us from making an incorrect diagnosis.” In order for us to understand a spinal related problem or any pain, we must not create a correct hypothesis, we must conclude an accurate diagnosis before we construct a prognosis and treatment plan. According to Frank Zolli, DC, the Dean of the University of Bridgeport College of Chiropractic for over 20 years, “every chiropractic student during their doctoral training learns at the most basic level of training that you must have an accurate diagnosis and then create a prognosis before you treat your patient.” Dr. Zolli continued by saying that this is taught in every CCE accredited chiropractic college.
Fiore in 2012 reported that accurate diagnosing was critical to the success of the chiropractic profession in order to be credible in the health care community. He also reported that many chiropractors hide behind the definition of chiropractic as the “…art, science and philosophy of locating and correcting nerve interference…” and continued on to say “This allows the chiropractic profession to have great latitude…but does not excuse us from making an incorrect diagnosis.” In order for us to understand a spinal related problem or any pain, we must not create a correct hypothesis, we must conclude an accurate diagnosis before we construct a prognosis and treatment plan. According to Frank Zolli, DC, the Dean of the University of Bridgeport College of Chiropractic for over 20 years, “every chiropractic student during their doctoral training learns at the most basic level of training that you must have an accurate diagnosis and then create a prognosis before you treat your patient.” Dr. Zolli continued by saying that this is taught in every CCE accredited chiropractic college.
 We also find there are many misperceptions about going all cash. Such as, going ALL cash means you are finally free to do what you want in making recommendations to all patients about their care. You can opt-out of every network and disregard terms of the PPO agreements. And, the BIG LIE many have heard is if you are all cash, you are immune to all the rules and regulations from your Board of Examiners, all the way up to CMS and the OIG, when it comes to proper documentation, billing, coding, discounting, state and federal inducement violations and other red tape including HIPAA.
We also find there are many misperceptions about going all cash. Such as, going ALL cash means you are finally free to do what you want in making recommendations to all patients about their care. You can opt-out of every network and disregard terms of the PPO agreements. And, the BIG LIE many have heard is if you are all cash, you are immune to all the rules and regulations from your Board of Examiners, all the way up to CMS and the OIG, when it comes to proper documentation, billing, coding, discounting, state and federal inducement violations and other red tape including HIPAA. 
