Defined, Trigenics® Myoneural Medicine is an energetic sensorimotor restoration system. It incorporates a neurologically-based, multimodal methodology for local or full-body assessment and treatment. Simplistically, it restores optimum brain and body communication and is directed at treating the causative, aberrant neurology of neuromusculoskeletal dysfunction. Aberrant histology (adhesions) and arthrokinetic osteology (subluxations) are then far more effectively treated using soft tissue myofascial techniques and joint manipulation procedures. Trigenics® can be applied as Western manual medicine to correct aberrant sensorimotor function or as Eastern meridian medicine to balance neurosomatic energetics.
Treatment procedures and outcome are based upon functional neurology. Trigenics® is not a soft tissue treatment technique, although the result of treatment using this technique is often the correction of many soft tissue conditions. From a manual medicine perspective, soft tissue myofascial techniques and osseous manipulation are still often needed to treat aberrant histology and arthrokinetic osteology. In some cases, Trigenics® works as a stand-alone system of care, although it is often used as an integral and critical component in a multidisciplinary approach to condition correction.
How Trigenics® Works
The myoneural procedures used involve the synergistic, simultaneous application of three main treatment techniques/modalities for a summative neurological effect: Reflex Neurology, Mechanoreceptor Manipulation and Cerebropulmonary Biofeedback. This mode of action works on the basis of integrating neurological convergence projection from both segmental (PNS) and suprasegmental (CNS) pathways. After reviewing the methodologies used in Trigenics, Dr. Ted Carrick, DC, PhD, DACAN, DABCN, DACNB, DAAPM, FACCN, and founder of the ACA neurology diplomate program, stated that “the multimodal stimulation approach utilized in Trigenics® is consistent with the principles of neuroplasticity and enhanced corticoneural reorganization of the somatosensory and sensorimotor systems.”
Trigenics® is used on a very wide variety of patients, including infants and geriatrics, and can be used to treat many conditions. In addition to being used to accelerate rehabilitation and for structural correction, it can be used as an alternative no-force manipulation. Specific Trigenics® Sports Power Augmentation treatments clinically increase athletic power and performance to greater than normal levels. Other neurological applications can be used for restrictive capsular and bursal conditions, such as “frozen shoulder”. Myoneural Exercises have also been developed to enhance patient recovery with neurologically enhanced exercise.
Trigenics® is often referred to as the “missing element” in neuromusculoskeletal care. In strictly using osseous manipulation to treat the vertebral subluxation complex, not correcting aberrant neurologic input (dysafferentation) to the muscular holding elements will lead to the frustrating outcome of chronic, recurring intervertebral dyskinesia. In treating musculoskeletal conditions, non-treatment of aberrant neural innervation and compensatory tone imbalances (short/weak muscles) will lead to the frustrating outcome of incomplete strength rehabilitation and functional restoration. Trigenics® provides the solution by firstly correcting aberrant proprioceptive neurology to provide for functional reafferentation and reefferentation. Treatment of aberrant histology (adhesions) and arthrokinetics (subluxation/dyskinesia) is subsequently addressed, using soft tissue myofascial techniques and chiropractic procedures.
Dystonia: A Case Study Using Trigenics® As the Primary Treatment
A 60-year-old male presented to the clinic on May 7, 2003, with complaints of bilateral neck discomfort over the two weeks prior. The neck pain was primarily acute right-sided upper trapezius, without radiation into his arm. The patient was also noticing increasing cervicogenic-type headache symptomatology into his right occipital area, with a tight hat-band feel at times. No recent trauma or accidents. In 1981, the patient was diagnosed, specifically, with adult-onset cervical dystonia myoclonic variant symptomatology. He also stated that it took the doctors and neurology specialists 15 years to reach that diagnosis. The patient feels better when he maintains an erect posture, and the symptoms of dystonia worsen when he turns his head to the right. The patient is currently medicated with clonazepam for the dystonia symptoms.
Dystonia Brief
Dystonia is a neurological movement disorder affecting more than 300,000 people in North America. It is characterized by involuntary muscle contractions, which force certain parts of the body into abnormal, sometimes painful, movements or postures.1 Its pathophysiology is complex and is not fully understood.2 Dystonia can affect any part of the body including the arms and legs, trunk, neck, eyelids, face, or vocal cords. It is not usually fatal, nor does it affect intellect. If dystonia causes any type of impairment, it is because muscle contractions interfere with normal function. Features such as cognition, strength, and the senses, including vision and hearing, are normal. Dystonia has numerous underlying etiologies,3 and is classified 3 ways: Age of onset, body distribution of symptoms or etiology. The classification of dystonia by etiology uses broad categories: Primary and secondary dystonia. Primary dystonia is defined by the existence of dystonia alone, without any underlying disorder. Secondary forms of dystonia arise from and can be attributed to numerous causes, such as birth injury, trauma, toxins, or stroke.
Physical Examination
Orthopedic testing was negative for any structural pathologies. Rhomberg’s, Houle’s, and Adson’s were also negative. Vibration sense, light touch and temperature were unremarkable. Cervical range of motion was digitally measured using a dual function hand-held inclinometer/dynanometer. Cervical range of motion findings are listed, comparing pre- and post-treatment measures. Manual muscle testing of the cervical and upper thoracic muscles was also digitally measured, using the MicroFET 3. The initial muscle strength test revealed equally bilateral weakness in nearly all the muscles tested. On the last re-evaluation, the testing was done prior to treatment.
Treatment
The patient was seen two-to-three times per week for 12 weeks. During each visit, the patient received 20 minutes of interferential nerve/muscle stimulation (IFC) on his cervical musculature, to relax muscles prior to the Trigenics® protocols. The patient met with the kinesiologist on a monthly basis for exercise therapy, which was primarily designed for daily home utilization. The patient was very diligent about keeping up with the at-home exercise regimen. Three months after his last treatment, the patient reported that he was continuing to do well with the following findings: Cervical flexion had more than doubled, going from 20 to 45 degrees; cervical extension had more than tripled, going from 10 to 35 degrees, left head rotation increased from 60 to 75 degrees; right head rotation almost doubled, going from 40 to 70 degrees; left lateral head flexion almost doubled, going from 20 to 35 degrees; and right lateral head flexion more than tripled, going from 10 to 35 degrees.
Digital muscle strength testing on the day of initial presentation of the cervico-thoracic musculature (including levator scapulae, upper trapezius, cervical extensor group, anterior scalenes, middle scalenes, sternocleidomastoid, suboccipitals, middle trapezius, rhomboids, pectoralis major middle head, pectoralis major lower head, pectoralis major upper head and pectoralis minor) revealed a summative strength measurement of 124.6 lbs of force on the right side of his body and 110.8 on the left side of his body. After 12 weeks of Trigenics® treatment, he had a summative measurement of 265.9 lbs on the right side and 220.0 on the left. This represents a 113.4% increase in his strength on the right side and 100% on the left.
Summary
Medical treatment of dystonia primarily relies on therapeutic agents, including anticholinergics, benzodiazepines, and botulinum toxin3 and neurofunctional surgery including deep brain stimulation.4,5
Trigenics® was recently redefined as a neuromanual sensorimotor restoration system.6 Its treatment protocols utilize a multimodal environmental stimulation, based upon a motoric window of change. It works on the basis of neurological convergence projection from both segmental and suprasegmental pathways. The myoneural procedures evoke a multimodal sensory motor activation at a rate specific to the patient, encouraging proper movement/muscle firing pattern, and beneficially altering the neurological input into the central nervous system. Home exercises are important to reinforce the treatments.
The aforementioned case study demonstrates dramatic clinical results using Trigenics® for increasing range of motion and functional strength in focal dystonia in the cervical region. In this case, significantly restricted ranges of motion were doubled or tripled. Also dramatic is the significant increase in strength, wherein the patient at least doubled his overall strength.
The brain can be guided to change its signal patterns through appropriate stimulation of the sensorimotor system. We look forward to further advancements and testing with other patients using the above and additional parameters. As chiropractic doctors, we have the skills and attainable knowledge to produce results such as these, without drugs or invasive measures.
References
1. www.dystonia-foundation.org
2. Trost M. Dystonia update. Curr Opin Neurol. Aug. 2003; 16(4):495-500.
3. Langlois M, Richer F, Chouinard S. New perspectives on dystonia. Can J Neurol Sci. Mar. 2003; 30 suppl 1:S34-44.
4. Kupsh A, Kuehn A, Klaffke S, Meissner W, Harnack D, Winter C, Haelbig TD, Kivi A, Arnold G, Einhaupl KM, Schneider GH, Trottenberg T. Deep brain stimulation in dystonia. J Neurol Feb. 2003; 250 Suppl 1:I47-52.
5. Lozano AM, Abosch A. Pallidal stimulation for dystonia. Adv Neurol 2004; 94:301-8.
6. Austin A. Lecture at the annual American Board of Chiropractic Sport Physician Symposium Mar. 2004, Las Vegas, Nevada.
Dr. James Fung is the Clinical Director of the Absolute Health Clinic in Toronto, Ontario, Canada. He received his undergraduate degree in Medical Genetics and Molecular Biology from University of Toronto and following that attended the Canadian Memorial Chiropractic College. For more information, visit www.absolutehealthclinic.com
A registered Trigenics Physician and Trigenics Instructor, Dr. Philip McAllister is the Clinical Director of the Back To Basics Chiropractic & Rehabilitation Centre in Guelph, Ontario, Canada, a multi-disciplinary center with the inclusion of Trigenics Myoneural Medicine. For more information, visit www.backtobasicscentre.com
Canadian-Estonian chiropractor, Dr. Allan Gary Oolo Austin, is the originator of Trigenics. Over 400 doctors and therapists throughout North America, Australia and Europe have now taken the Trigenics RTP program. For more information, call 1-888-514-9355 or visit www.trigenicsinstitute.com.

 Chiropractic care is essential for the pregnant mother. Her systems and organs are now providing for two, and their optimal function is critical for the baby’s healthy development. The mother’s spine and pelvis undergo many changes and adaptations to compensate for the growing baby, and the risk of interference to her nerve system is substantially increased. Specific chiropractic care throughout pregnancy works to improve nerve system function, providing greater health potential for both the mother and baby.
Chiropractic care is essential for the pregnant mother. Her systems and organs are now providing for two, and their optimal function is critical for the baby’s healthy development. The mother’s spine and pelvis undergo many changes and adaptations to compensate for the growing baby, and the risk of interference to her nerve system is substantially increased. Specific chiropractic care throughout pregnancy works to improve nerve system function, providing greater health potential for both the mother and baby.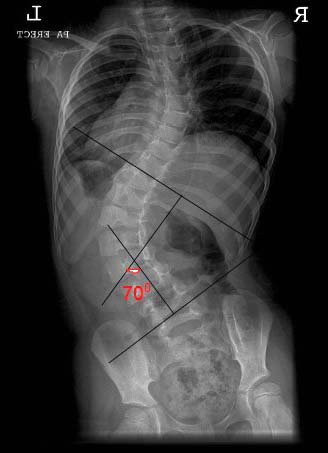
 Dr. Hugh B. Logan, who founded Logan College of Chiropractic, first developed the basis for this procedure for the correction of scoliosis. Over the last fifty years, I have modified, improved and updated the procedure to allow the chiropractor to produce consistent results. I established the International Scoliosis Research Center to provide research, consultation and seminars to the profession on this subject. The doctor of chiropractic is the only health care professional capable of reducing a scoliosis without braces or surgery.
Dr. Hugh B. Logan, who founded Logan College of Chiropractic, first developed the basis for this procedure for the correction of scoliosis. Over the last fifty years, I have modified, improved and updated the procedure to allow the chiropractor to produce consistent results. I established the International Scoliosis Research Center to provide research, consultation and seminars to the profession on this subject. The doctor of chiropractic is the only health care professional capable of reducing a scoliosis without braces or surgery.