The knee has an impressive level of stability, despite the incongruent joint surfaces of the tibia and femur. These two contrasting joint surfaces articulate only with the help of the crescent-shaped menisci. Through their weight-distribution and shock-protection properties, the menisci help guide movements between the convex surfaces of the distal femur and the almost flat superior surfaces of the tibial plateau.
A second knee joint involves articulation between the femur and patella. The integrity of this joint is dependent on the coordinated contraction of the quadriceps muscles and the proper positioning of the patella on the saddle-shaped femoral surface. Normal knee-joint movement includes pivot flexion and extension, with external tibial rotation on the femur during the last 10-to-20 degrees of extension.1
Unfortunately, conditions that produce excessive rotation of the tibia relative to the femur make the knee susceptible to the development of several degenerative conditions.
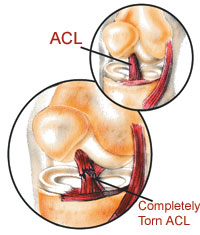
The anterior cruciate ligament (ACL) prevents excessive anterior glide displacement of the tibia on the femur, hyperextension, and internal tibial rotation. A review of normal and abnormal biomechanics of the gait cycle reveals why ACL injuries are among the most common ligamentous injuries of the knee.2
The Foot/Knee Connection
Pronation of the foot in the contact period helps to absorb shock, and it is normally accompanied by internal rotation of the tibia relative to the femur. Excessive pronation during gait will transmit damaging forces up the kinetic chain. It is the excess of these rotational forces which result in repetitive microtraumas. If this conversion of torque, in response to pronation, occurs beyond normal limits, the tibia can subluxate in internal rotation.
The most common cause of degenerative joint disease is the presence of abnormal biomechanical forces on a normal or healthy joint. The next most common situation is the application of normal forces on abnormal cartilage. Excessive pronation, which causes internal tibial fixation and stretches the ACL, creates the necessary ingredient for both of these processes to occur simultaneously.
In their study comparing measurable drop of the navicular due to pronation with the incidence of ACL injury, Beckett, et al., found the injured subjects had higher navicular drop scores.3 The results are summarized in Table 1.
|
|
Table 1. Navicular Drop Scores |
|||
|
Group |
Number of Participans |
Right Foot |
Left Foot |
|
|
The.anterior.cruciate.ligament (ACL)prevents.excessive anterior.glide.displacement of.the.tibia.on.the.femur, hyperextension,.and internal.tibial.rotation. |
1. ACL uninjured | 50 | 6.9+/ -3.2 |
6.9+/ -2.8 |
| 2. ACL injured | 50 | 13.0+/ -4.4 |
12.7+/ -4.0 |
|
In another study, Loudon, et al., measured postural faults as predictors for the occurrence of non-contact ACL injury. Seven postural positions were measured: pelvis, hip, sagittal knee, frontal knee, hamstring length, ankle pronation, and navicular drop test. Postural distortions—including knee hyperextension, excessive navicular drop, and excessive pronation—were significant predictors for ACL injury.4
Remember that knee pain can often precede visual radiographic evidence of degeneration. The navicular drop test can be a good preventative screening tool.
Adjust, Support, Rehabilitate
Conservative care for non-traumatic knee pain and degeneration should include:
· adjustments—to provide proper alignment and remove restricted motion (especially internal tibial rotation fixation)
· orthotic support—to control excessive pronation and internal tibial rotation
· rehabilitative exercise—to build the muscles and improve stability
Custom-made, flexible orthotics support the bones and soft tissues of the feet in their proper position of function. By correcting pedal imbalances (which can cause excessive pronation and tibial torsion), orthotics help prevent overuse injuries and knee-joint degeneration. Research published in the Journal of Manipulative and Physiological Therapeutics proves that custom-made orthotics improve the structural alignment of the foot, thereby creating a more symmetrical foundation throughout the entire kinetic chain.5 Further research has shown that custom-made, flexible orthotics decrease (normalize) the Q-angle and improve patellar tracking. This indicates an improved functional alignment of the knee and leg.6
Developing muscles helps stabilize the joint and lower the incidence of serious knee injury.7 Rehabilitative exercises—including strengthening and coordinating contraction of muscles involved in flexion, extension, and rotation—will help enable the patient to perform a range of movements to build strength in muscle groups interacting with the knee. TAC
Dr. John J. Danchik is the seventh inductee to the American Chiropractic Association Sports Hall of Fame. He is the current chairperson of the United States Olympic Committee’s Chiropractic Selection Program. He lectures extensively in the United States and abroad on current trends in sports chiropractic and rehabilitation. Dr. Danchik is an associate editor of the Journal of the Neuromusculoskeletal System. He has been in private practice in Massachusetts for 26 years. You can contact him at: [email protected]
References
-
Logan AL. The Knee: Clinical Applications. Gaithersburg, MD: Aspen Publishers, Inc.; 1994.
-
Bergfeld J, et al. Injury to the anterior cruciate ligament. Phys Sportsmed 1982; 10:47-59.
-
Beckett ME, et al: Incidence of hyperpronation in the ACL injured knee: a clinical perspective. J of Athletic Training 1992; 27(1):58-62.
-
Loudon JK, Jenkins W, Loudon KL. The relationship between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther 1996; 24(2):91-97.
-
Kuhn DR, Shibley NJ, Austin WM, Yochum TR. Radiographic evaluation of weight-bearing orthotics and their effect on flexible pes planus. J Manip Physiol Ther 1999; 22(4):221-226.
-
Kuhn DR, Yochum TR, Cherry AR, Rodgers SS. Immediate changes in the quadriceps femoris angle after insertion of an orthotic device. J Manip Physiol Ther 2002; 25(7):465-470.
-
Roy S, Irvin R. Sports Medicine Prevention, Evaluation, Management and Rehabilitation. Englewood Cliffs, NJ:Prentice-Hall; 1983.