Thirty Percent of Intervertebral Disc Herniations Are Missed on MRI
by Dr. William J. Owens, D.C., D.A.A.M.L.P.
Diagnostic: attentiveness has always been a hallmark of accurate trauma assessment. The diagnostic dilemma relates to finding the traumatic lesion, and clinically correlating it to causality and, when appropriate, to persistent functional loss. There may be a single, straight forward answer to subjective complaints, or there may be a more subtle presentation that may involve several pain generating structures concurrently. The clinical examination is the most important step in determining the traumatic lesion, the patient’s diagnosis, treatment plan and subsequent prognosis.
diagnostic dilemma relates to finding the traumatic lesion, and clinically correlating it to causality and, when appropriate, to persistent functional loss. There may be a single, straight forward answer to subjective complaints, or there may be a more subtle presentation that may involve several pain generating structures concurrently. The clinical examination is the most important step in determining the traumatic lesion, the patient’s diagnosis, treatment plan and subsequent prognosis.
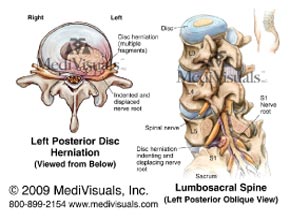
The article that is being reviewed was published in SPINE. This study was a collaborative effort between the Department of Orthopedic Surgery, The First Affiliated Hospital of Soochow University, China, and the Department of Orthopedic Surgery, UCLA, Los Angeles, CA. This manuscript was designed to review the accuracy of traditional MRI studies in the diagnosis of lumbar intervertebral disc herniation. The authors cite a study that was published in the journal Radiology in 1995 showing that, in cases of acute lumbar radiculopathy, only 70% of the patients that were diagnosed with a lumbar disc herniation based on clinical examination had a lumbar disc herniation confirmed by MRI. That obviously means, 30% of patients with a disc herniation do not show that herniation on traditional MRI studies.
That is where the concept of the functional lesion comes into being. Once they are out of the initial acute inflammatory phase, many trauma patients will describe the pain varying throughout the day and with specific activities. These differences are generally based on the position and biomechanics of the spine, such as walking up or downstairs, standing or sitting. They can also vary based on the time of day, which indicates that water content of the disc is an influencing factor in the generation of pain. Structural continuity of the spine is an important factor, as different positions will have different effects on spinal anatomy.
The following list may assist you in connecting the dots in relation to the lumbar spine and functional positioning:
1. Lumbar extension – loads the posterior elements of the spine (facet joints) and decreases the size of the intervertebral foramen.
2. Lumbar flexion – increases intradiscal pressure and is associated with sitting and standing.
3. Lateral flexion – take either of the above positions and induce a lateral flexion component and you will also compress neural elements on ipsilateral side. This will also increase intradiscal pressure at the lateral aspect of the disc and compress the facet joint complex on that side.
These important concepts are the basis for this entire article, since cases where there is limited association between diagnostic testing and clinical symptoms have perplexed clinicians for a long time. The authors stated, “Flexion and extension radiographs and computed tomography myelography were the standard methods of obtaining positional images of the spine. However, because MRI yields an image that is superior to radiographs and less invasive than myelography, physicians have been experimenting with ways of using MRI to obtain positional images of the spine.”1
This brings us to the concept of functional MRI studies. The article utilized an MRI with vertical orientation of the opposing magnet donuts, allowing scanning of the patient in an upright axially loaded position. That is an interesting concept and set up; however, many areas of the country do not have that luxury, so we may need to work these concepts into studies, using traditional recumbent MRI. The fascinating part of this paper was that, not only were more intervertebral disc lesions visualized and, therefore, diagnosed, but also those that were present, increased in size when provocative positions were implemented. Imaging patients in the position of most pain has been a helpful addition into solving the diagnostic dilemma. The authors wrote, “A significant increase in the degree of lumbar disc herniation was found by examining flexion and extension views when compared with neutral views alone.”2
The results of the study showed:3
1. For patients with normal or 3mm bulge in extension and 15.29% demonstrated an increase to >3mm in flexion.
2. Patients in the neutral view that had baseline disc pathology of 3 to 5mm, 13.28% had increased herniations to >5mm in extension and 8.47% had increased herniation to >5mm in flexion.
3. For patients with baseline disc pathology of 5 to 7mm in neutral, 10.58% increased in extension and 5.78% increased in flexion. In addition, for patients with a baseline disc pathology of 7 to 9mm in neutral, 9.09% increased in extension and 4.55% increased in flexion.
Orthopedic testing in the office is nothing more than provocative testing of injured structures. This approach should be implemented into our advanced imaging procedures in trauma to insure the traumatic lesion is identified in a timely manner. Looking to functional positioning during MRI evaluations, especially in the lumbar spine, should be a part of every clinician’s diagnostic protocols.
 In each issue, a clinical topic is covered by William J. Owens of the American Academy of Medical Legal Professionals (AAMLP), which is a national, non-profit organization, comprised of doctors and lawyers. The purpose of the organization is to provide its members with current research in trauma and spinal related topics, to keep the profession on the cutting edge of healthcare. Members may also sit for a Diplomate examination and be conferred a DAAMLP. The organization also offers support to the individual member’s practice.
In each issue, a clinical topic is covered by William J. Owens of the American Academy of Medical Legal Professionals (AAMLP), which is a national, non-profit organization, comprised of doctors and lawyers. The purpose of the organization is to provide its members with current research in trauma and spinal related topics, to keep the profession on the cutting edge of healthcare. Members may also sit for a Diplomate examination and be conferred a DAAMLP. The organization also offers support to the individual member’s practice.
To learn more or join, go to www.aamlp.org or call 1-716-228-3847.
References:
1) Zou, et al., 2008, ppE142
2) Zou, et al., 2008, ppE142
3) Zou, et al., 2008, ppE140