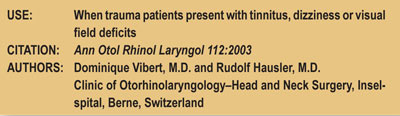
Vestibular Deficits after Whiplash Injuries
by William J. Owens, D.C., D.A.A.M.L.P. & Mark E. Studin, D.C., F.A.S.B.E.(C), D.A.A.P.M., D.A.A.M.L.P.
This manuscript addresses one of many important issues to keep in mind when evaluating patients that present with neck or head trauma. In the case of whiplash type injuries, it is the inertia of the trauma that causes the injury. The context of this paper was relative to whiplash injuries without direct head trauma; however, any type of acceleration/deceleration syndrome can produce symptoms of tinnitus, dizziness or visual field deficits (falls, fights, contact sports). It is reported that “dizziness and vertigo are reported in 25 percent-50 percent of [whiplash] cases.”
When evaluating a patient that complains of the above symptoms, in what ways do you strive to objectify those subjective complaints? Determining the proper diagnostic test will assist you in a proper and timely medical specialty referral.
In this paper, the authors reviewed three individual cases where the patients had experienced acute peripheral vestibular dysfunction following car accidents. The following cases were discussed and, as you can see, the speed and collision type varies.

1: Case #1: “Fifty-seven-year-old male, frontal collision, speed approx 100km/hr.”
2: Case #2: “Twenty-two-year-old female, rear-end collision, speed approx 60km/hr.”
3: Case #3: “Fifty-six-year-old woman, lateral collision, speed approx 50km/hr.”
Most importantly, “Lesions of the vestibular organs, particularly the otolithic organs after whiplash injuries, are probably underestimated by attributing dizziness and vertigo symptoms mainly to cervical damage and lesions of the central nervous system.” They also stated in the article that “otolithic dysfunction seems not to be directly correlated to the severity of the whiplash injury”.
It was determined that these types of symptoms can be found in all five categories of whiplash injury; therefore, it is most important to evaluate the patient properly to obtain an accurate diagnosis.
Two tests that are specific to these injuries and subjective complaints include:
1. Brainstem Auditory Evoked Potential (BAEP): This test, as the name implies, targets the brainstem area and is a recording of the electrical activity coming from the brain stem.
2: Electronystagmography (ENG): Electronystagmography is a test to look at voluntary and involuntary eye movements.
It evaluates the acoustic nerve, which aids with hearing and balance.
The paper also references that Oosterveld, et al., 1991, “demonstrated that of 262 patients investigated six months to five years after a whiplash injury, 85 percent complained of persistent dizziness such as rotary vertigo (50 percent of cases), and 35 percent complained of erroneous body sensations (floating sensations). Tinnitus was present in 14 percent of patients and unilateral or bilateral hearing loss was reported in 5 percent of cases.

Finally, it was stated that, “Lesions of the vestibular organs, particularly the otolithic organs after whiplash injuries, are probably underestimated by attributing dizziness and vertigo symptoms mainly to cervical damage and lesions of the central nervous system. A complete otoneurological examination should be undertaken as soon as possible after the accident, that is, within the first days to weeks.
Each issue, a clinical topic will be provided by Drs. Mark Studin & William J. Owens of the American Academy of Medical Legal Professionals (AAMLP), which is a national non-profit organization comprised of doctors and lawyers. The purpose of the organization is to provide its members with current research in trauma and spinal-related topics to keep the professional on the cutting edge of healthcare. Members may also sit for a Diplomate examination and be conferred a DAAMLP. The organization also offers support to the individual member’s practice. To learn more, go to www.aamlp.org or call 1-716-228-3847.