Depression Era Marketing for Today
by Mark R. Payne D.C.
O kay…so, I said it. The dreaded “D” word. The pundits may debate whether our economy is in recession or a true depression but, if you’re out there trying to survive this economic mess, I suspect that technical distinctions don’t matter much. Fact: If chiropractors can’t figure out a way to serve their patients and survive this financial downturn, a whole bunch of us won’t be here a year from now. That sounds like a depression to me.
I talk to lots of doctors and things are tough all over. But don’t lose sight of the fact that times are tough on your patients right now, too. The fact that they are losing their jobs doesn’t change one thing about whether or not they need your care. Regardless of their economic circumstances, people still need your help. They’re still in pain, still sick, and still depending on you.
With that in mind, I want to relate something from my first quarter in chiropractic college—something that stuck with me and is just as relevant now as ever. Fall of 1976, the college was all abuzz about a famous doctor from Wisconsin who was visiting the campus. As a dumb freshman, the name didn’t mean anything to me, but everyone else seemed impressed, so I went to listen. For about an hour, the older gentleman shared his insight on treating patients and how he managed to grow a thriving practice during the throes of the great depression. The doctor was Clarence Gonstead.
It was 1929, and a terrible flu epidemic was in full swing. In some towns, as much as thirty percent of the population was sick at any given time. More than 50,000 people died in the winter of 1928-29 from flu and related pneumonia…more deaths than in the entire Vietnam War. Dr. Gonstead worked his Mt. Horeb clinic six and a half days a week from early morning until late evening. Very sick patients were often seen multiple times daily. Mrs. Gonstead would often bring lunch so he could treat patients straight through the day. On Fridays and Saturdays, he would close the office, go home for a quick supper and be back to open the doors at 10:00 PM for folks who were exiting the “picture show” and wanted to stop by for an adjustment while they were in town.
There was no such thing as health insurance and no one but the patients to pick up the bill. But, still, they came. Unemployment was approaching twenty percent, but patients still referred their friends and relatives. In a rapidly deflating economy, dollars were in very short supply and, yet, they still valued the service enough to part with much needed cash.
And Dr. Gonstead wasn’t the only chiropractor to survive and flourish during the depression. There were nearly eighty chiropractic colleges operating by 1930 and many doctors did quite well, considering the bleak economy. But, of course, success was measured by a different set of standards then. There were no such things as a BMW or Lexus, no dreams of a new mansion in a gated community, no expectations of working three days a week and retiring at fifty. Doctors were quite happy with a dependable Ford, a modest home in a decent part of town, and enough money at the end of a long week to support their families. Hard work was the order of the day and Dr. Gonstead was as good an example as this profession ever had.
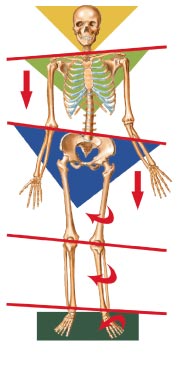
Were there other factors responsible for pushing the Gonstead clinic and chiropractic to uncommon success during tough times? Perhaps. For one thing, professional fees had to be affordable for the patients. For another, chiropractic promoted a simple, understandable model of health care…a simple bone out of place pinching a nerve. True, that old single bone model of subluxation is now outdated, but the old acronym of K.I.S.S. (Keep It Simple, Stupid) is just as relevant as ever. That’s one of the things I love most about practicing around a “posture paradigm.” It allows me to communicate with patients in factual, yet very simplistic, language. Patients can see and understand postural imbalance when they view it in a mirror or on an X-ray.
Chiropractic was founded around the “unique selling proposition” (little bit of marketing lingo there) of the relationship between spinal structure and bodily function. That simple, understandable concept played a central role in the rapid growth of the profession. Things are quite different now. Most chiropractors can’t explain succinctly what they do; the doctor-patient relationship has been complicated by third party pay plans, and most new doctors can’t imagine working twelve hour days, or making a house call for a sick child. They work nine to five, take a three hour lunch, and keep their home phone numbers unlisted.
Are you struggling to survive in today’s economy? I would submit that, in some respects, building your practice today isn’t really all that different than in the Great Depression. It still makes sense to communicate with patients in simple terms they can understand. Hard work and frugality are still at the heart of success. Finally, making your services affordable and becoming an example of service-based leadership within your community will do more to build your reputation than any marketing gimmick or management seminar. As it turns out, even in the midst of a depression, patients can still spot a doctor who really has their best interests at heart.
 Dr. Mark Payne is the president of Matlin Mfg., a manufacturer and distributor of postural rehab products since 1988. To request more information on managing the scoliotic patient with postural chiropractic methods, call 1-334-448-1210 or link to
Dr. Mark Payne is the president of Matlin Mfg., a manufacturer and distributor of postural rehab products since 1988. To request more information on managing the scoliotic patient with postural chiropractic methods, call 1-334-448-1210 or link to
www.MatlinMfg.com








 S
S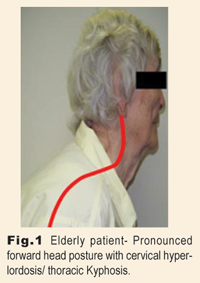



 Stynchula’s method (AKA “Compression-CounterStressing” Traction) has also been studied and found to be essentially equal to compression traction in terms of restoring the cervical lordosis.2 Advantages include patient comfort, space efficiency, and ease of use. Fig. 2 shows the method in use. Compression-CounterStressing Traction is ideal for use in the professional office and also serves well as a backup method for home use, if patients can’t handle the Dakota Traction (See Fig. 1)
Stynchula’s method (AKA “Compression-CounterStressing” Traction) has also been studied and found to be essentially equal to compression traction in terms of restoring the cervical lordosis.2 Advantages include patient comfort, space efficiency, and ease of use. Fig. 2 shows the method in use. Compression-CounterStressing Traction is ideal for use in the professional office and also serves well as a backup method for home use, if patients can’t handle the Dakota Traction (See Fig. 1)