BUT … and there’s always a but … because she was now going the alternative care route and incurring out of pocket cost, the question she posed to me that afternoon was “Is there an insurance plan that covers these treatments?” I replied, “That is a very good question, my friend. Let me check into it and get back to you.”
That was 1998. The concept of insurance that covered alternative wellness care seemed brilliant. I began an exhaustive search across the country and back, to find any insurer anywhere that would cover natural treatments for a diagnosed illness, beyond the usual minimal coverage for massage, chiropractic visits, and infrequent acupunture.
The result of my search? Zilch ! Not even one insurance plan existed. I found one union self-funded plan in California that covered more natural wellness modalities than insurance did, but you had to be a union worker living in California to participate. My search came to a dead end. And tremendous disappointment. Why not, I wondered. Why didn’t such a plan exist?
I began formulating in my mind what an insurance plan should look like, if it were to cover natural and alternative health care treatments. This came easier for me than it might have for an agent with a typical health insurance background, for two reasons:
1) One consequence of my going ‘above and beyond’ for clients was making enough ruckus to get the attention of people other than front line customer service stiffs, who answer the phones at Big Insurance. I was tolerated by staff members involved in the meat – underwriting, actuary, claims, etc. I ended up absorbing health insurance’s inner workings.
2) I had a long time aversion to traditional western medicine and, at the time, a 17-year history of successfully self treating my own family’s occasional illnesses via nutritional methods.
The two backgrounds gave me the basis for what was to become Aegis Insurance Solutions. As time passed, the idea became more than a daydream … I jotted notes whenever a brainchild manifested, and began organizing them.
Meanwhile, as the turn of the century arrived, I watched health insurance deteriorate from a once utile product into an increasingly unaffordable, increasingly gutted, barely recognizable shell of its original format. Premiums climbed at an alarming pace to keep up with skyrocketing claims experience.
Health care costs, escalating at 500% of normal inflation, threatened to bankrupt the country. Actuaries predicted that health care would gobble 1/5 of the country’s entire GDP by the year 2013, if trends didn’t change. Health care surprised even the actuaries by beating projections two full years, usurping one in every five dollars spent in the U.S. by the end of fiscal 2011. How is that even possible ?
Well, for starters, over the last decade traditional medical care providers have driven claims costs (translate insurance premiums) through the roof with outrageously priced, ineffective treatments. Add to that prescription drug prices which increase quarterly, since Congress lifted the ban on television drug advertising in the late 1990s.
Insurance companies fought hard to contain costs by eliminating covered services, increasing deductibles and co-pays, increasing premiums, etc. They got tough on network fee schedules and lost significant network provider membership as a result. Meantime, insurance premiums tripled anyway since 1998. And an ever increasing population (near 50 million at last count) goes uninsured. The national healthcare forcemeat, Obamacare, has zero power to tame the monster because it has zero provision for cost containment.
It became painfully evident that something had to be done to reverse health care trends because insurers were literally drowning in costs. Health insurance companies began jumping ship in droves at the turn of the century, realizing there was simply no way to be profitable anymore. And consumers suffered.
Compare consumer choices for health insurance today with the 1990s versions. Insurance agents in that era offered clients a selection of health plans from dozens of insurers. Competition was fierce to provide the best benefit package for the smallest price. Ten years later, the choice of insurers shrank to a half dozen. Benefits vanished, premiums grew unaffordable, employers dropped coverage. Yet Obamacare’s solution is to compel people who can’t afford coverage to buy it anyway, or pay a hefty penalty.
Believe it or not, insurance companies laid the ground work for today’s disaster by unintentionally eliminating personal responsibility for health care decisions and spawning over-utilization of benefits. How on earth did they accomplish all that? By implementing plans in the mid 1980s that covered almost unlimited medical care for minimal co-pays.
One could logically ask how insurers could make a mistake with such profoundly disastrous consequences. It evolved almost overnight, due to fear. Cancer shock-loss claims were increasing at an alarming rate, with no upper end in sight. And despite new admonitions by the American Cancer Society about the importance of early detection via preventive screening, Average Jill refused to undergo screening because she had to pay for it. Insurers desperately needed a plan to encourage early diagnosis, to slow the avalanche of new cancer claims.
So insurers caved and came up with first dollar insurance coverage as incentive for obtaining preventive care. They couldn’t have anticipated how quickly policyholders would develop a new mentality – “Why should I care how much my healthcare costs?” “I pay ten bucks for a doctor visit. Instead of buying Desitin for the baby’s rash, I’ll take her to a pediatrician and get a prescription.”
Insurers inadvertently created an insurance gremlin that mutated into a monster before they had the first inkling of the damage it would do. But that’s just part of the story. Western healthcare practitioners are not without huge blame for the crisis that evolved. They have more than a decade of experience now, gouging insurance companies at every opportunity.
Example – doctors once required annual office visits to reauthorize a patient’s prescription. But when insurance began first dollar coverage, doctors began requiring that patients show up quarterly to get the same prescription reauthorized. After all, the patient had little out of pocket cost – no sweat off his back!
Some doctors identified opportunities to become real estage magnates at the expense of insurers (translate–premium dollars paid by you and me.) They erected labs and free-standing surgical facilities, rather than rent privileges at the local hospital, because they could bill insurance to cover the new mortgages while increasing their net worth. Doctors began ordering endless streams of unecessary tests and performing unnecessary surgeries to generate fees, since patients didn’t have to pay. Buildings got built while dollars poured into coffers like water roaring over a dam.
Because I believe that a higher standard of ethics exists in the natural wellness arena of the healthcare universe, it was a surprise to watch even wellness practitioners make an occasional grab for a slice of the new insurance pie. My own massage therapist charged self-pay clients $65 per hour and historically refused to accept insurance. But now she decided to accept insurance because she could bill $150 for people injured in vehicle accidents – providing the exact therapy I received at $65 per hour. During one visit, she bragged about her newfound wealth.
Make no mistake, I understand a fair charge to cover the cost of generating a bill. Billing and waiting for payment costs money. But charging 130% over the fee for cash clients isn’t fair. After seven years of routine therapy, I was suddenly compelled to find a new massage therapist.
A local chiropractor charges cash patients $35-$65 per (follow-up) adjustment visit, based on ability to pay – admirable. But he bills insurance $120 for the same visit – not admirable, not fair, not ethical. That drives up the price of MY health insurance.
Recently I stumbled into an insurer’s worst nightmare. I used a Groupon to try a local massage therapist for the first time. Massage therapy is so beneficial I’ve opted to self pay for routine visits the past fifteen years. In addition to monthly visits, I make a point to obtain treatment from new therapists often, especially when traveling. It keeps my neck and shoulders from tightening up, after dozing in uncomfortable seats hours on end. (Thai massage is best so far!)
:dropcap_open:Hospitals bill insurance 300-500% over actual cost of providing care and, for some services, even 1000% mark-up.:quoteleft_close:
After my massage therapy was complete (excellent work), I considered scheduling another round. The desk clerk inquired if I’d had massage therapy before. I replied, “hundreds of times.” She asked if had insurance she could bill. I informed her there was nothing wrong with me – no diagnosis. She then lowered her voice to inform me that the doctor could create a diagnosis. I could come in for more frequent massages, paid by insurance. I was astounded.
Not only did she encourage me to cheat my insurer by submitting a fraudulent claim. She was clueless as to the fact that ANY diagnosis affects my future insurability for years, and maybe even permanently. Not just health insurance, but disability income insurance, life insurance, long term care insurance, etc. She could do me lasting harm by falsifying a diagnosis.
Astonishment gave way to disgust. I held my tongue and left, but I won’t go back. Note to self – that practitioner will not be part of the Aegis provider network.
I’ve related how so many allopathic practitioners and even some natural wellness practitioners contributed to today’s crisis in U.S. health insurance. But when we examine the contribution from privately owned hospitals, we discover they are greedier – by light years – than any individual practitioner. Hospitals bill insurance 300-500% over actual cost of providing care and, for some services, even 1000% mark-up. Consider too that these are supposedly not-for-profit organizations !
The federal government allows hospitals 4-5% over cost under existing national health care (Medicare). Medicare determined that a not-for profit entity can cover cost and make a reasonable profit at that reimbursement schedule. Yet, in fiscal 2005-06, a group of seven U.S. catholic hospital systems in the southwest netted a profit of over $2 billion (and all in the name of Christ). No income taxes due, no sales taxes due, no property taxes due – zero taxes on two billion dollars. Hospitals more than make up for stingy government pay schedules by gouging private insurance. And they laugh all the way to the bank, while your insurance premiums spiral and your benefits shrink.
After nearly 20 years of battling the monster that insurers birthed with first dollar coverage plans in the mid 1980s, health insurance companies are still at a loss as to how to even begin to bring it under control, much less how to reverse damage done. They’re fresh out of ideas and have no clue what to do next.
Aegis does! And ironically, the solution is first dollar coverage! Sound ludicrous? It isn’t, when you know what we know. The ONLY solution to greed in traditional health care, to outlandish insurance premiums, to a shrinking selection of insurance plans, is a first dollar insurance plan which promotes natural wellness and alternative treatment. It’s so simple it’s brilliant – the ONLY way to fix the mess is to facilitate good health.
Why does that work? Because making someone well brings an end to insurance claims. Claims become finite, rather than chronic, lifelong, and increasingly expensive.
A good side effect – because natural wellness is nondestructive, the body suffers no damage. Thus it averts potential additional costs associated with treatment of bad side effects that often result from dangerous allopathic methods. Even the most oblivious insurance underwriter understands that if you heal a man, instead of just treating him, you put a finite dollar amount on that man’s claim, which eventually results in reduced insurance premiums.
Increasing numbers of enlightened patients today prefer treatment with more effective alternative methods, but insurance won’t pay. When patients can’t afford self-pay, what are their options? None. They revert back to traditional care that insurance WILL pay for. So by refusing to pay for alternative natural treatments, traditional insurance perpetuates the problem it desperately wants to resolve. More doctor visits, more tests, more procedures, more drugs, more side effects – same routine, same results. People remain ill … claims experience continues to accelerate.
Health insurers not only can’t fix it – they exacerbate the dilemma of spiraling claims experience by encouraging over-utilization through faulty plan design. With the health insurance crisis becoming an unbearable burden on the financial resources of this country, our alternative insurance plan is the only logical, viable, long term solution. Our plan solves ALL current problems in health insurance:
First, we don’t accept bills from practitioners. Every insured pays for his care at time of service, and then submits his own claim for reimbursement. Thus we eliminate the need for our provider members to hire staff to track insurance billing and make it possible for them to charge a universal fair fee for service rendered. Requiring patient payment for service also restores personal responsibility for the cost of the patient’s health care, by making him aware that there is a price for unwellness – that there is indeed a correlation between his personal financial health and his lifestyle choices.
Second, we don’t negotiate fees with our network providers, making membership in our network desirable. This creates excellent choices for our insured members when they need care. We prefer a network replete with the best practitioners, so insureds have access to the very best wellness care. When you’re the best, you’re worth what you charge. Your patient/client gets well – our customer’s claims costs are finite.
Third, we make it financially appealing for our insured members to seek natural wellness instead of consulting traditional practitioners because we want them to get well – not to be in treatment. Because we make it inexpensive for members to obtain natural care and (very) expensive for them to obtain allopathic care, we control the cost of care. In the end, reduced cost always means lower premiums.
Fourth, in the employer group health arena, we actually refund large chunks of premium at the end of a plan’s fiscal year to insured employers whose group health plan design encourages employee wellness. Their claims costs are dramatically lower than employers who fail to differentiate between traditional care and natural treatments. So we offer handsome rewards to employers who help improve the bottom line.
Until now, Aegis has offered coverage only to employer groups. But the winds of change are blowing. In the near future we’ll introduce an individual insurance plan in most states, which covers the full spectrum of natural and alternative treatments. Of course we include coverage for traditional care when it’s required. If you fall off your bike and break your arm, we wouldn’t penalize you for practicing healthy living.
 :dropcap_open:W:dropcap_close:hat is the chiropractic profession’s position when it comes to treating scoliosis? What have our chiropractic universities taught us? Are we only treating subluxations and not the scoliosis? Are we adjusting for symptoms and not trying to correct the scoliosis? Why does the scoliosis patient live if there are extreme subluxations?
:dropcap_open:W:dropcap_close:hat is the chiropractic profession’s position when it comes to treating scoliosis? What have our chiropractic universities taught us? Are we only treating subluxations and not the scoliosis? Are we adjusting for symptoms and not trying to correct the scoliosis? Why does the scoliosis patient live if there are extreme subluxations? 

 Concerns surrounding chiropractic office employee training escalated from what is known as “incident to” concerns, which stemmed from the interests of third-party payers who were being billed for services performed by office employees that did not have documented training. In 2008 the American Chiropractic Association (ACA) and the Federation of Chiropractic Licensing Boards (FCLB) asked the postgraduate subcommittee of the Association of Chiropractic Colleges (ACC) for recommendations surrounding chiropractic employee training to help address this issue.
Concerns surrounding chiropractic office employee training escalated from what is known as “incident to” concerns, which stemmed from the interests of third-party payers who were being billed for services performed by office employees that did not have documented training. In 2008 the American Chiropractic Association (ACA) and the Federation of Chiropractic Licensing Boards (FCLB) asked the postgraduate subcommittee of the Association of Chiropractic Colleges (ACC) for recommendations surrounding chiropractic employee training to help address this issue. 
 As healthcare providers, we have the important job of making sure we listen to patients, administer the proper care and relieve patients’ pain so they start to feel better again. Our goal is to help them perform as optimally as possible and it involves teamwork between the doctor and the patient. We guide patients in healing, while they must, in turn, do their home care and perform any exercises we recommend.
As healthcare providers, we have the important job of making sure we listen to patients, administer the proper care and relieve patients’ pain so they start to feel better again. Our goal is to help them perform as optimally as possible and it involves teamwork between the doctor and the patient. We guide patients in healing, while they must, in turn, do their home care and perform any exercises we recommend. 
 If you’ve been spending hours on the treadmill and not seeing any results, it’s because long distance cardiovascular exercise can decrease testosterone and raise your stress hormone levels like cortisol1. Increased levels of cortisol stimulate the appetite, increase fat storage, and slow down or inhibit exercise recovery.
If you’ve been spending hours on the treadmill and not seeing any results, it’s because long distance cardiovascular exercise can decrease testosterone and raise your stress hormone levels like cortisol1. Increased levels of cortisol stimulate the appetite, increase fat storage, and slow down or inhibit exercise recovery.
 One Florida afternoon I was doing my utmost to provide excellent service for the client sitting across from me. I’d chided her for months, every time we met, about her ongoing reliance on Mayo Clinic doctors for health care that was costing her a fortune and wasn’t doing any good. Today I was pleased to learn that she was paying attention, finally. She’d been consulting a natural wellness practitioner whom I’d recommended and reported that she was noticing a difference. I mentally patted my back.
One Florida afternoon I was doing my utmost to provide excellent service for the client sitting across from me. I’d chided her for months, every time we met, about her ongoing reliance on Mayo Clinic doctors for health care that was costing her a fortune and wasn’t doing any good. Today I was pleased to learn that she was paying attention, finally. She’d been consulting a natural wellness practitioner whom I’d recommended and reported that she was noticing a difference. I mentally patted my back.
 Due to the fact that this is about contracts and contract law, there are many ways to interpret the language within those contracts. Lawyers hired by the insurance companies have made a “cottage industry” out of using the courts to redefine the agreements to secure additional profits. The carriers have been so successful that they have retained some of the best firms nationally to ensure increasing profits. The carriers are now utilizing “old” technology created for their benefit with a twist to further increase their bottom line at your expense: IMEs and Peer Reviews.
Due to the fact that this is about contracts and contract law, there are many ways to interpret the language within those contracts. Lawyers hired by the insurance companies have made a “cottage industry” out of using the courts to redefine the agreements to secure additional profits. The carriers have been so successful that they have retained some of the best firms nationally to ensure increasing profits. The carriers are now utilizing “old” technology created for their benefit with a twist to further increase their bottom line at your expense: IMEs and Peer Reviews. 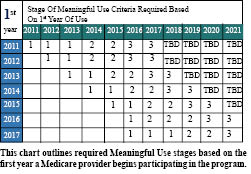
 Under the proposed rules, providers were to progress to Stage 2 Meaningful Use criteria after two program years of meeting Stage 1 criteria. For example, Medicare providers who first demonstrated Meaningful Use in 2011 would need to meet Stage 2 criteria in 2013. CMS has now delayed the onset of Stage 2 criteria so that the earliest a provider would have to demonstrate Stage 2 criteria is 2014.
Under the proposed rules, providers were to progress to Stage 2 Meaningful Use criteria after two program years of meeting Stage 1 criteria. For example, Medicare providers who first demonstrated Meaningful Use in 2011 would need to meet Stage 2 criteria in 2013. CMS has now delayed the onset of Stage 2 criteria so that the earliest a provider would have to demonstrate Stage 2 criteria is 2014.
 Physicians must report on three of six Menu-Set Objectives:
Physicians must report on three of six Menu-Set Objectives:
 Dr. Lee was known for his chiropractic expertise in the field of sports injury. He wrote countless articles on the topic, especially those related to running. He was a seminar speaker for Foot Levelers, Inc., for more than 15 years. He brought not only knowledge and experience to these seminars but also his warmth, humor and compassion. He conveyed more than words on a PowerPoint slide to his students; he taught them by his actions how to find the good in every situation, in every person, every day. His optimism and gratitude cannot be forgotten. He always found a way to make someone laugh or charm them with his sense of style or brighten their day with a kind word. He knew that being a chiropractor was more than being a healer and used his profession to help others not only with his hands but also with his words and actions.
Dr. Lee was known for his chiropractic expertise in the field of sports injury. He wrote countless articles on the topic, especially those related to running. He was a seminar speaker for Foot Levelers, Inc., for more than 15 years. He brought not only knowledge and experience to these seminars but also his warmth, humor and compassion. He conveyed more than words on a PowerPoint slide to his students; he taught them by his actions how to find the good in every situation, in every person, every day. His optimism and gratitude cannot be forgotten. He always found a way to make someone laugh or charm them with his sense of style or brighten their day with a kind word. He knew that being a chiropractor was more than being a healer and used his profession to help others not only with his hands but also with his words and actions.
 In the use of good quality lumbar bracing that is approved by Medicare (the only ones I will use) it is important to document in the patient’s chart why the brace is given and its effectiveness. A physician must and should expect good results and the chart should reflect those results.
In the use of good quality lumbar bracing that is approved by Medicare (the only ones I will use) it is important to document in the patient’s chart why the brace is given and its effectiveness. A physician must and should expect good results and the chart should reflect those results.
 This article will walk you through the uncertain economic maze and give you clear-cut strategies you can utilize so, no matter what happens to insurance, you will be in a profitable position to deliver great chiropractic care to your patients.
This article will walk you through the uncertain economic maze and give you clear-cut strategies you can utilize so, no matter what happens to insurance, you will be in a profitable position to deliver great chiropractic care to your patients.