Dr. Larry Wilkins, Founder and Director of Laurel Mountain Chiropractic Clinic in Mt. Pleasant, PA, has added post-graduate hours in such studies as rehabilitation, manipulation under anesthesia, nutrition, pediatrics, exercise, and advanced work in the Pierce Chiropractic Method.
As an involved professional, Dr. Wilkins has many accomplishments to his credit. He has served as a board member of two chiropractic organizations in Pennsylvania for eight years. Also, he is a teacher of the Pierce Chiropractic Method, and worked very closely with Dr. Vern Pierce until his death.
Dr. Wilkins is also the founding member of two very prestigious chiropractic organizations—Metro Chiropractic Services and the Chiropractic Golden Circle. In addition, he was nominated and accepted into the Chiropractic Knights of the Round Table in 1983.
In an interview with The American Chiropractor (TAC), Dr. Larry Wilkins (Wilkins) describes his successful career in chiropractic and the recent addition of axial decompression to his practice.
TAC: What inspired you to become a chiropractor?
Wilkins: It all began for me when I was a junior in high school. My uncle, Wilmer McGiffin, had a brother-in-law, Dr. Don Casteel, who was a chiropractor. My uncle and my father thought I would make a good chiropractor, even though I had absolutely no idea what that was or meant. So, they took me to Palmer College for a tour of the campus. I got a good feeling about the campus, and decided to give it a try!
After graduation from high school in 1969, I enrolled in Palmer College, and completed my education in June 1973. After my first quarter at Palmer College I was hooked on chiropractic. It has been my life’s work and passion ever since.
TAC: What has really impacted your growth as a chiropractor and that of your practice?
Wilkins: In 1974, I met Dr. Vern Pierce who quickly took me under his wing and proceeded to teach me what Palmer College had not and that was the philosophy of chiropractic. Most of the chiropractors who speak on the subject of philosophy were taught by B. J. Palmer, as was Vern. Now, it seemed that most chiropractors either hated B. J. or loved B. J., and it really doesn’t matter to me, because the bigger issue is this: the only thing that we have, that all other health care practitioners don’t, is our philosophy!
Vern was one of the greatest influences on my life; he taught me his technique, philosophy, and how to run a chiropractic office.
TAC: What type of patients do you generally treat or attract?
Wilkins: The types of patients we attract into our practice are crisis-care patients, low back pain, headaches, neck pain, sick people, and some wellness patients. We have been slowly changing this; our ideal practice would be a cash practice full of wellness patients, on the chiropractic side, and then, chronic and sub-chronic patients on the decompression side. These would be patients with bulging discs, herniated discs, degenerative disc disease and failed back surgeries.
We attract a wide variety of patients to the practice. For a very long time, I was like the “country doctor.” The patients would come to me with everything and ask my opinion about all their health care needs. The reason for this, I believe, is because I practice in a small town of 6,500 people and eight other chiropractic offices. I have, through chiropractic care, assisted two hundred women in getting pregnant; I have gone to patients’ homes in the middle of the night when their children were turning blue because of the croup. I adjusted them, and before I could watch most of the movie that the parents were watching, the child was breathing normally! In thirty-three years of practice, no child I have ever adjusted died of SID’s, and I know the reason why.
I have helped people dying of cancer or other systemic diseases pass away with grace and very little pain, and before you ask, yes, they were also under the care of a medical doctor.

TAC: What are your specialties?
Wilkins: If I do have a specialty it would be the certain something that B. J. always spoke of: I give everyone of my patients hope. Then, along with the hope, I use every ounce of knowledge I have gained through all the previous patients whom I have treated. Add to that all the things I have learned over the course of thirty-three years, and that would be my formula for patient care.
At this point, I would have to also say the Pierce technique and the use of the PulStarFras adjusting instrument were my only techniques, until recently finding decompression along with the DRS™ protocol of axial decompression.
We use axial decompression on chronic patients. Also, we use the Pierce technique, which is excellent for correction of hypolordotic and military cervical curves. I get the kind of results that drive patients here just from talking to my current patient base. The patients love axial decompression because it is gentle and highly successful, and they can’t get that at other practices or through other methods like drugs and physical therapy.
TAC: What made you decide to add axial decompression to your practice?
Wilkins: My reason for adding decompression work to our clinic was that I hated to see patients that were visibly in pain with low back or cervical spine disc conditions being marginally helped with only chiropractic care. After great research, I found the axial decompression treatment to help them. What impressed me was the fact that I could help someone no one else was able to help. Plus the fact that I could help people with failed surgeries. It still amazes me the severe and chronic cases that respond. And it amazes me how easily it truly works. We had a patient that had a surgery on his low back that caused his left leg to become totally numb for fifteen years. After only ten sessions of axial decompression, his foot was warm and he had some feeling for the first time in fifteen years. No words can express how he felt or how grateful he was.
TAC: How has axial decompression impacted your practice?
Wilkins: We have greatly enlarged the patient base that we can help. For instance, people with degenerative disc disease, herniated and bulging discs, facet syndrome, and failed back surgery syndrome can now be helped with the work we do with decompression. A lot of my patients have no other solution to their problems except surgery. They have tried muscle relaxors, pain pills, anti-inflammatories, physical therapy, epidurals, cortisone injections, oral steroids—with little or no relief. About twenty-five percent of our patients have had one, two or three spinal surgeries with no help, and then they turn to our office and axial decompression. In most cases, we have been able to help them enjoy a pain free life.

It truly has been a miracle for many of our patients who had no hope, and before decompression we wouldn’t have been able to help them!
TAC: Do you have any extraordinary patient success stories that you would like to share with us?
Wilkins: Two cases I would like to discuss, were both very unique and unusual, to say the least.
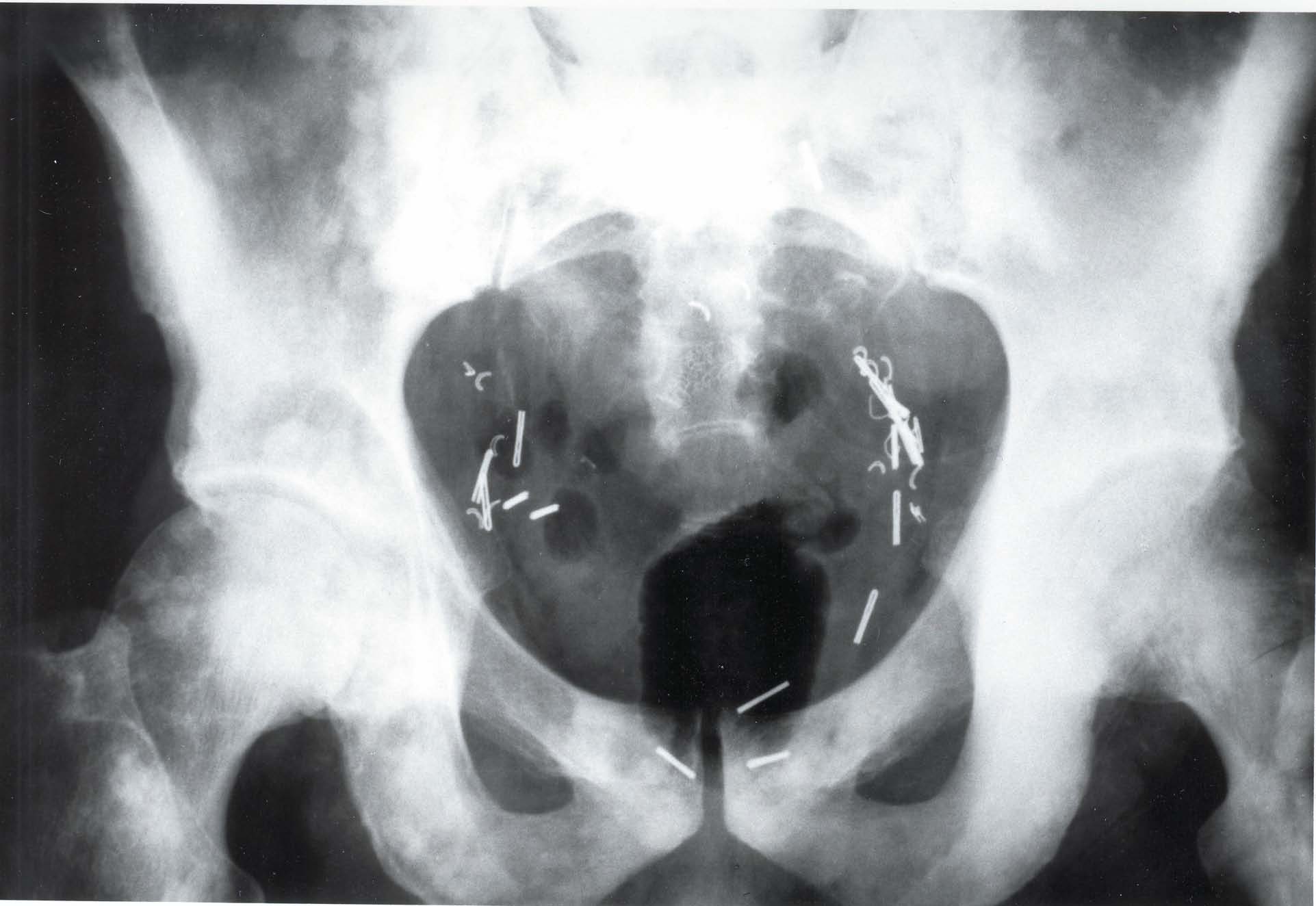
The first one, Sandy, came to me with a fusion of the lumbar vertebra with metal plates and screws. I knew there were contraindications, but this lady was persistent. Being a person of great love and caring for people, I decided to try to help her. Long story short, we treated her very slowly. The results were short of a miracle. After ten sessions, she went from having to have her husband and me pull her out of a chair to getting out of the chair herself, with ease. I have followed her case, and after two years she is still doing great. In fact, she speaks to prospective patients on the phone to answer any questions they may have about axial decompression and my office!
The second patient is Vivian. She had three spinal surgeries and, with the last one, a morphine drip was placed surgically inside her with a tube going into the disc. She also was in a great deal of pain. She also traveled quite a distance to see me, but her results were just as impressive as Sandy’s. Her neurosurgeon spoke with her and told her it would be okay for me to do axial decompression, and that I could even treat the disc in which the morphine drip was placed.
I was not very comfortable with that, so I chose another disc level and went to work. She responded extremely well to the care. However in her case, the treatment took longer than it would have for the average patient. Not unexpectedly, it took thirty-one treatment sessions to get her 85 percent improved. The patient went from hardly being able to walk to spending long hours on her husband’s motorcycle. Unfortunately, I won’t be able to track the longevity of her case, because twelve months after care, Vivian passed away. Vivian was struck by a blood clot that went from the lung into the heart. Her husband made a special and touching trip to my office to tell me how great Vivian’s last twelve months were without her crippling intense pain.
These two cases are the very reason I offer axial decompression in my office.
TAC: How do your patients pay?
Wilkins: Almost 98 percent of my decompression practice is cash. This is a great time to tell you why. If the patients have a vested interest in their health, they will naturally do much better with care than if someone else is responsible for it. But the biggest reason is what a patient said to me the other day, “If you had not made me pay for the service, I would probably have quit before I got the results I could have!”
I believe that having a great understanding of running a cash practice or a partial cash practice will be the difference of being in practice in the future, rather than not being in practice.
TAC: What single piece of advice would you give a new chiropractor just starting out?
Wilkins: In my heart, the answer to the question of advice for a new chiropractor just starting out would be two-fold, and in no particular order. The one that has always been with me came from Dr. Pierce and Dr. Gonstead; it was to be the master of one technique. By doing that, you are going to be proficient enough to treat 90 percent of the people coming in your door. You will have a reason for everything you do with regard to chiropractic. The second would be to sign up with a practice consultant.
TAC: What general advice would you give an established chiropractor whose practice might be struggling?
Wilkins: If you are looking for growth as a chiropractor, the easiest way I have found is to find a great coach. In my lifetime, I have had fantastic coaches. The first was Dr. Vern Pierce, who taught me a great adjustment technique and the philosophy of chiropractic.
The next coach that came into my life was Dr. Chuck Gibson. He taught me all the great procedures for running an office and managing patients—not in a clinical context, but in maintaining control, and educating the patients as to why they were there.
Another great coach was Dr. C. J. Mertz. He taught me how to do what Dr. Pierce and I had wanted to do for years and could not figure out how. That was how to care for the patients the way we wanted to—not the way the insurance companies wanted us to—and get paid for it.
When I became involved with axial decompression, I also needed a coach. For this, I researched and chose Freedom Awaits™. Dr. Richard E. Busch, III and Dr. Jack Ashton not only taught me how to use decompression properly, but also how to do it with love, passion, caring and ethics.
TAC: Any final words for our readers?
Wilkins: I can honestly say that there is nothing else in the world that I would rather be doing than chiropractic and axial decompression. Our profession is so very easy to do. You just have to have the right knowledge, and if you don’t have the right knowledge it is readily available; all you have to do is find the doctor that will teach you. I have mentioned five of them. Seek them out, and pick their minds. Don’t waste a precious moment of your life.There are too many patients that need you to help them achieve optimum health. These two quotes by Vince Lombardi sum it up best: “The difference between a successful person and others is not a lack of strength, not a lack of knowledge, but rather in a lack of will;” and, “The quality of a person’s life is in direct proportion to their commitment to excellence, regardless of their chosen field of endeavor.”
You may contact Dr. Wilkins at 724-547-5030, 724-547-3377, or email [email protected].
 The patient enters your office and has significant pain radiating into an extremity. Being responsible, you adopt the policy of the insurers and treat the patient conservatively for 4-8 weeks and the pain doesn’t diminish; you then refer the patient to the imaging company for an MRI.
The patient enters your office and has significant pain radiating into an extremity. Being responsible, you adopt the policy of the insurers and treat the patient conservatively for 4-8 weeks and the pain doesn’t diminish; you then refer the patient to the imaging company for an MRI.